The Future of IPAA Treatment: Is Endoluminal Vacuum Therapy the Answer?
"A pilot study reveals promising results for endoluminal vacuum-assisted therapy in treating anastomotic leaks after ileal pouch-anal anastomosis (IPAA), potentially reducing the need for surgery and improving patient outcomes."
Anastomotic leaks following ileal pouch-anal anastomosis (IPAA) can lead to significant complications, impacting functional outcomes and potentially causing pouch failure. Traditionally, treatment has involved surgical interventions to address these leaks, but a new approach is gaining traction.
A recent pilot study published in Techniques in Coloproctology explores the use of endoluminal vacuum-assisted therapy (EVT) as a primary treatment for anastomotic leaks after IPAA. The study investigates whether EVT alone can effectively manage these leaks without the need for additional surgical procedures.
This article will delve into the findings of the study, examining the methodology, results, and implications for the future of IPAA leak management. By understanding this innovative approach, patients and healthcare professionals can make more informed decisions about treatment options and improve patient outcomes.
How Does Endoluminal Vacuum Therapy (EVT) Work for IPAA Leaks?
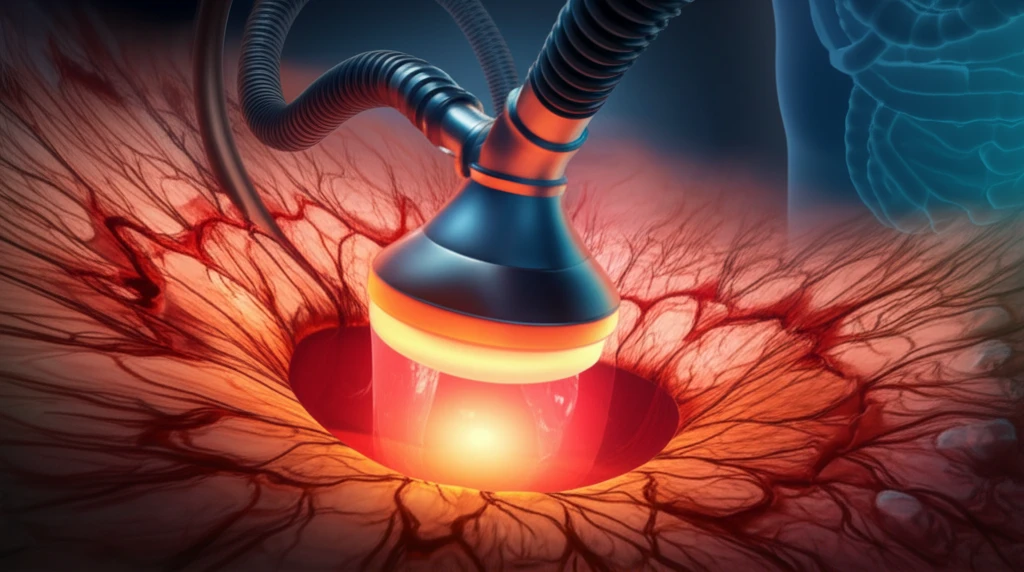
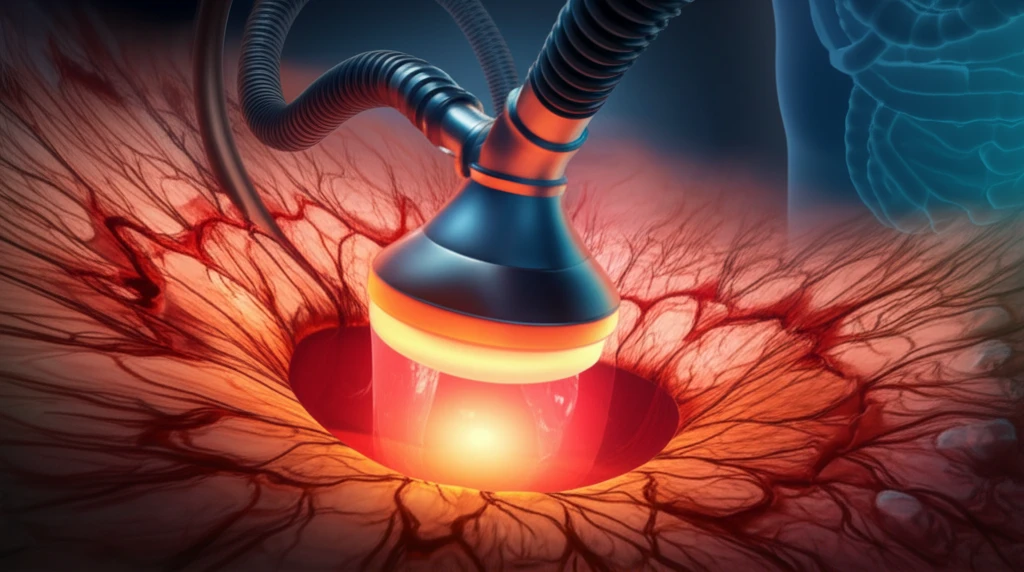
Endoluminal vacuum therapy involves placing a specialized sponge, known as Endosponge®, directly into the anastomotic leak cavity. This open-pored polyurethane sponge is connected to a vacuum suction bottle, which creates continuous negative pressure within the cavity. This negative pressure facilitates several key processes:
- Fluid Drainage: The vacuum suction effectively removes contaminated fluids and debris from the leak cavity, reducing the risk of infection and promoting a cleaner environment for healing.
- Cavity Reduction: The continuous suction helps to collapse the leak cavity, gradually reducing its size over time.
- Granulation Tissue Formation: The negative pressure stimulates the growth of healthy granulation tissue, which fills the cavity and promotes closure of the leak.
A Promising Step Forward in IPAA Leak Management
The results of this pilot study offer a promising outlook for the use of Endosponge® therapy in managing anastomotic leaks after IPAA. The study suggests that EVT can be an effective primary treatment option, potentially reducing the need for more invasive surgical interventions. However, it is important to acknowledge that this was a pilot study with a limited number of patients, but EVT shows potential as a valuable tool in the management of this challenging complication.
