The Future of Dental Implants: Combining Tech for Better Bone Growth
"New research shows how combining titanium mesh with a special membrane can significantly improve bone regeneration for dental implants, leading to better outcomes."
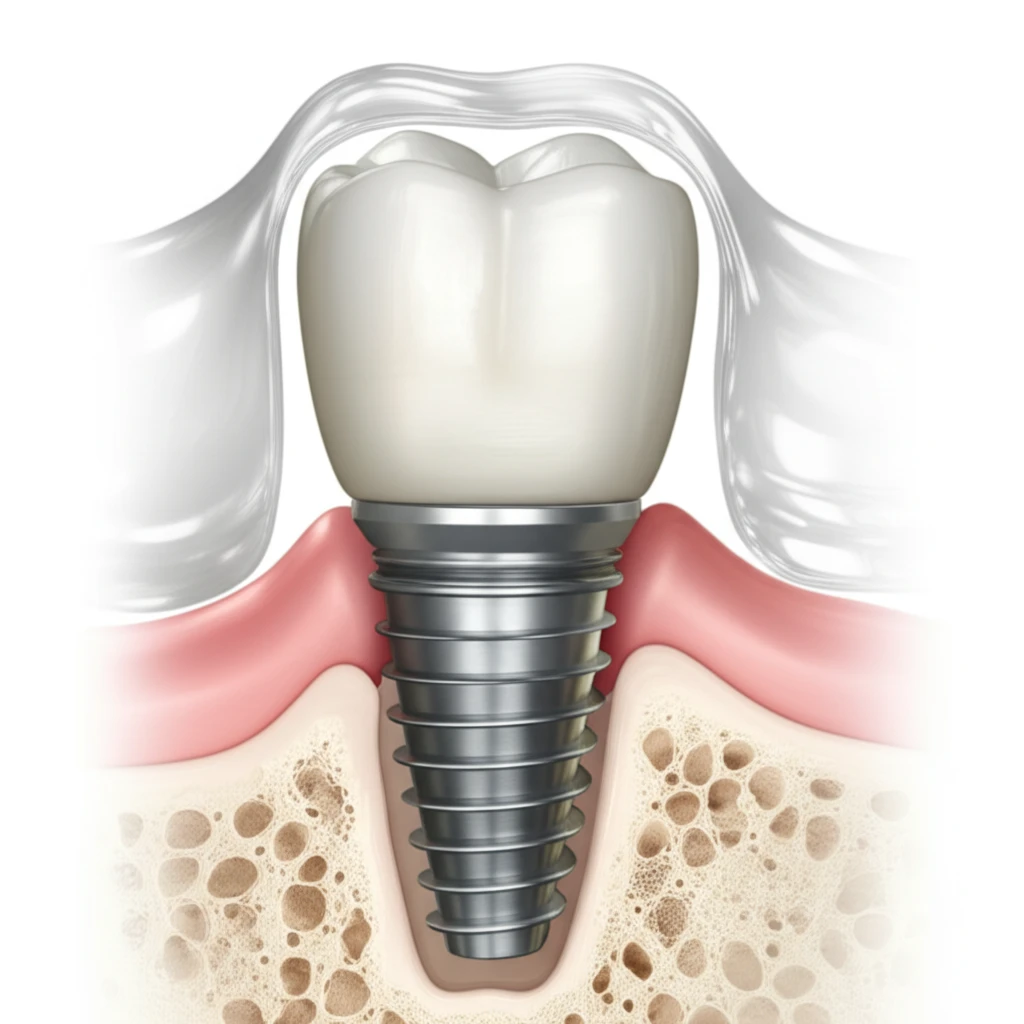
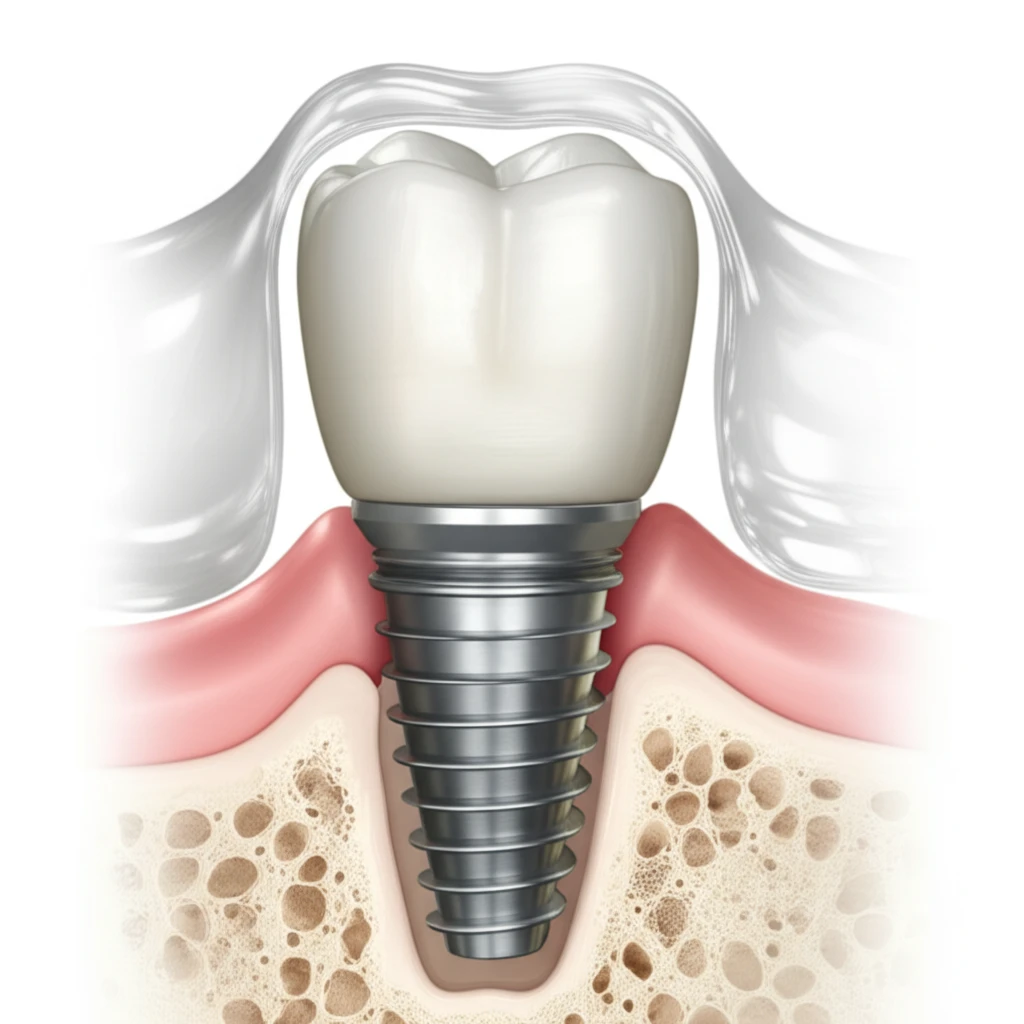
For anyone considering dental implants, a key factor for long-term success is having enough healthy bone to support the implant. Unfortunately, bone loss can occur due to various reasons, making it difficult to place implants properly. That's where guided bone regeneration (GBR) comes in, aiming to rebuild bone where it's needed.
GBR involves using membranes to create a protected space around the implant site, preventing soft tissue from interfering with bone growth. While GBR has shown promise, researchers are constantly exploring ways to enhance its effectiveness. Now, a recent study investigates a combination approach that could revolutionize how we address bone defects in dental implant procedures.
This article will dive into the findings of this research, explaining how combining titanium mesh with a special collagen membrane (Bio-Gide) can lead to significantly improved bone regeneration compared to using either material alone. We'll explore the potential benefits of this approach and what it could mean for the future of dental implant surgery.
Why Combining Titanium Mesh and Bio-Gide Could Be the Key to Implant Success
Researchers set out to evaluate the effectiveness of different membrane combinations for GBR in beagle dogs. They created alveolar bone defects (bone loss around where implants would be placed) and then used three different treatment approaches:
- Group A: Implant + Bio-Oss (a bone grafting material) + Titanium mesh
- Group B: Implant + Bio-Oss + Bio-Gide membrane
- Group C: Implant + Bio-Oss + Titanium mesh + Bio-Gide membrane
What This Means for the Future of Dental Implants
This study suggests that combining titanium mesh and Bio-Gide membrane offers a promising approach for repairing alveolar bone defects and improving the success of dental implants. The combination appears to provide enhanced bone regeneration compared to using either material alone, potentially leading to more predictable and stable implant outcomes.
While this research was conducted on beagle dogs, the findings provide a strong rationale for further clinical studies in humans. If these results translate to human patients, this combination approach could become a standard of care for GBR in dental implant surgery.
For those considering dental implants, it's essential to discuss bone regeneration options with your dentist or oral surgeon. This research highlights the importance of innovative techniques and materials in achieving optimal bone support for long-term implant success. Ask your provider if combination techniques such as this one might be appropriate for your specific case.
