The Future of Autoimmune Treatment: How Killer Artificial Antigen Presenting Cells (KaAPC) Could Revolutionize Therapy
"Discover how KaAPC offers a precise, efficient way to deplete harmful T cells in autoimmune diseases, offering a potential alternative to broad immunosuppression."
Current treatments for autoimmune diseases often rely on broad immunosuppression, which, while managing symptoms, can lead to significant side effects such as increased susceptibility to infections and malignancies. This underscores the urgent need for more targeted therapies that can precisely address the root causes of these conditions without compromising the entire immune system.
In recent years, cell-based immunotherapy strategies have emerged as promising alternatives. These approaches often involve using antigen-presenting cells (APCs) to modulate the immune response. However, traditional methods can be technically challenging and may not always be effective due to their sensitivity to cytotoxic T cell responses.
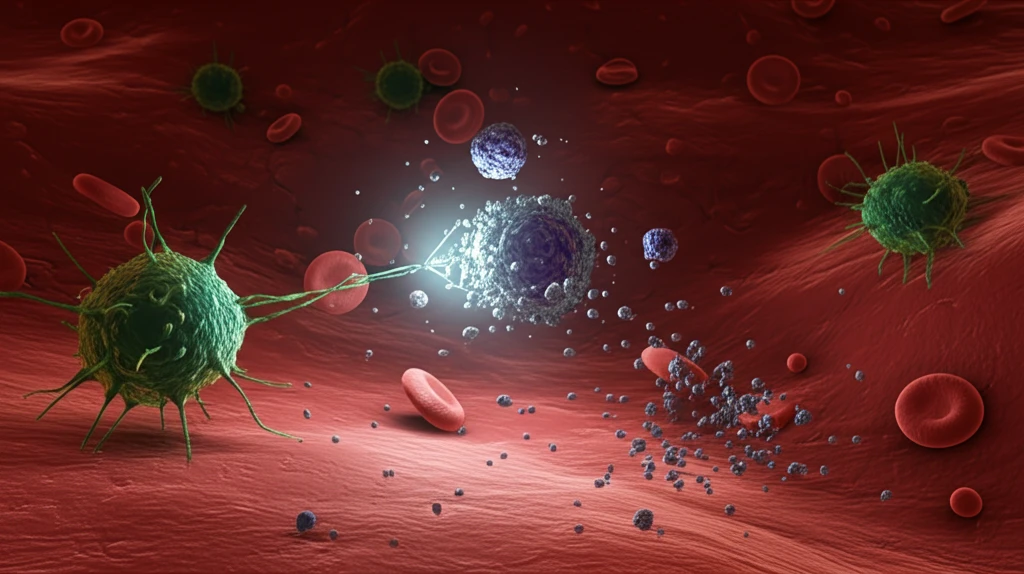
Killer Artificial Antigen Presenting Cells (KaAPC) offer a novel solution by enabling the targeted depletion of pathologic T cells while preserving the broader immune system's functionality. This innovative approach holds considerable promise for treating autoimmune diseases and preventing allograft rejections by specifically regulating undesirable T cell responses. This article delves into the mechanics, benefits, and potential future applications of KaAPC technology.
What are Killer Artificial Antigen Presenting Cells (KaAPC)?
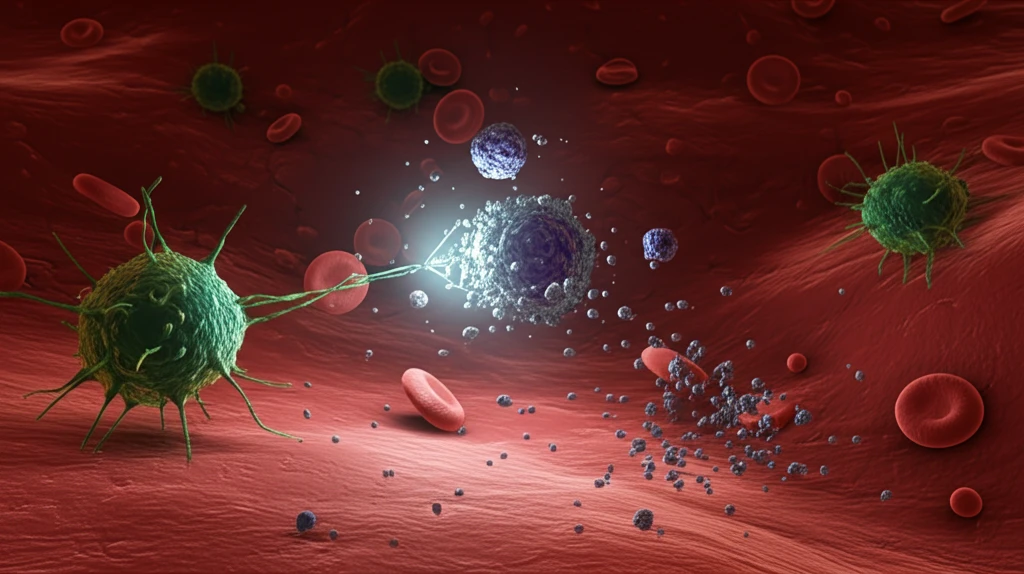
Killer Artificial Antigen Presenting Cells (KaAPC) are synthetically engineered constructs designed to mimic the function of natural antigen-presenting cells, but with enhanced precision and control. Unlike traditional cell-based therapies, KaAPC are non-cellular, bead-based systems that can be easily manufactured and standardized. They consist of a HLA-A2-Ig dimer (signal 1) and an anti-Fas mAb (apoptosis-inducing signal) covalently immobilized onto a surface of a 4.5 µm paramagnetic latex bead.
- Precision Targeting: KaAPC selectively target and eliminate disease-causing T cells.
- Preservation of Immune Function: The broader immune system remains untouched, maintaining its ability to fight infections.
- Ease of Production: As a non-cellular system, KaAPC can be easily manufactured and standardized.
- Dual-Action Mechanism: KaAPC presents antigens to T cells while delivering an apoptosis signal.
The Future of KaAPC Therapy
KaAPC represent a significant advancement in the field of immunotherapy, offering a targeted and efficient way to modulate T cell responses in autoimmune diseases and other conditions. While the current research is primarily focused on in vitro applications, the potential for in vivo use is substantial. Future studies may explore the use of biocompatible or biodegradable matrices to enhance KaAPC's applicability in clinical settings. By continuing to refine and expand this technology, researchers hope to develop new and more effective treatments for a wide range of immune-related disorders.
