The Curious Case of the Wandering Bullet: What Happens When a Projectile Takes a Detour?
"A medical mystery unfolds as a bullet embarks on an unexpected journey through the circulatory system, highlighting the importance of thorough trauma assessments."
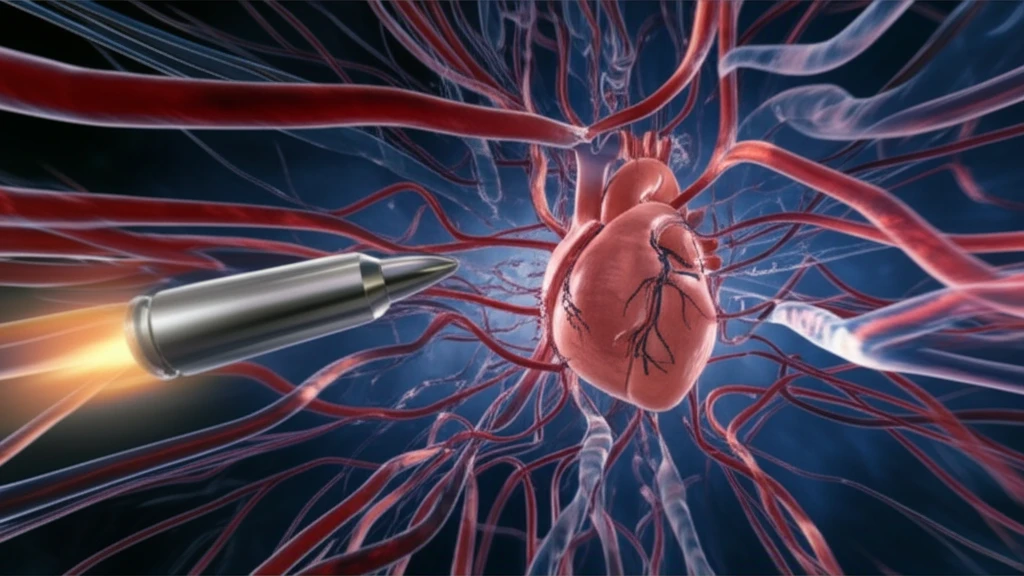
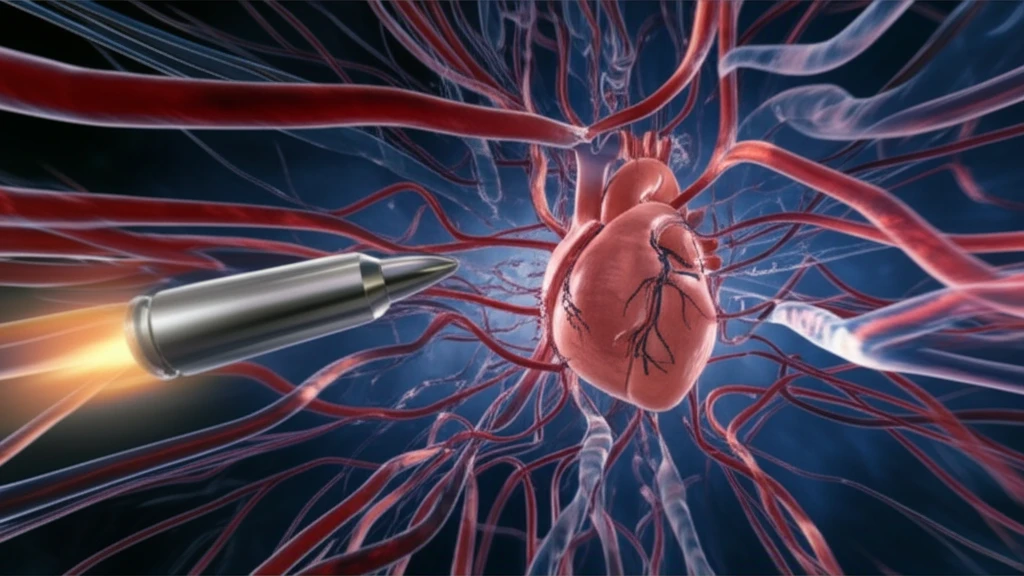
Imagine a bullet, not just piercing through tissue, but embarking on a journey through the body's intricate network of blood vessels. This rare phenomenon, known as venous embolization, occurs when a foreign object, like a bullet, enters the vasculature and travels to distant sites. While it's an uncommon complication of penetrating trauma, its potential consequences demand a heightened awareness among medical professionals.
The incidence of bullet migration into the vasculature is estimated to be around 0.3%. Although seemingly low, the morbidity associated with such emboli can be as high as 25%. This means that a significant number of patients who experience this complication face serious health risks. The decision to remove these errant bullets remains a subject of debate within the medical community.
This article delves into a fascinating case report that illustrates the complexities of venous embolization. By examining this real-life scenario, we'll explore the diagnostic challenges, treatment considerations, and the importance of meticulous follow-up in patients with penetrating trauma.
From Wound to Wonder: Tracing the Bullet's Path
A 20-year-old male arrived at the Emergency Department with multiple gunshot wounds. Initial assessments revealed entry points in his extremities, but no foreign bodies were immediately apparent in the lower limbs. However, a chest radiograph, prompted by the proximity of the wounds to the thoracic cavity, unveiled a surprise: two metallic foreign bodies. One near the left humeral head, and another in the central mid-thoracic region.
- Initial Assessment: Multiple gunshot wounds, prompting thorough examination.
- Unexpected Findings: Chest radiograph reveals foreign bodies in the thorax.
- Diagnostic Imaging: CT scan pinpoints bullet location in the right ventricle.
Lessons Learned: Navigating the Complexities of Bullet Embolization
This case underscores the challenges and controversies surrounding the management of bullet emboli. While recommendations exist for retrieval versus conservative management, the decision must be individualized based on the patient's symptoms, risk factors, and the bullet's location.
The role of interventional radiology is also evolving. Their expertise in endovascular retrieval techniques offers a less invasive alternative to traditional surgery. As this case demonstrates, the ability to adapt to a moving target is crucial in managing bullet emboli.
Ultimately, this case serves as a reminder of the importance of a meticulous approach to trauma care. From the initial physical exam to long-term follow-up, vigilance and a broad differential are essential in ensuring the best possible outcome for patients with retained foreign bodies.
