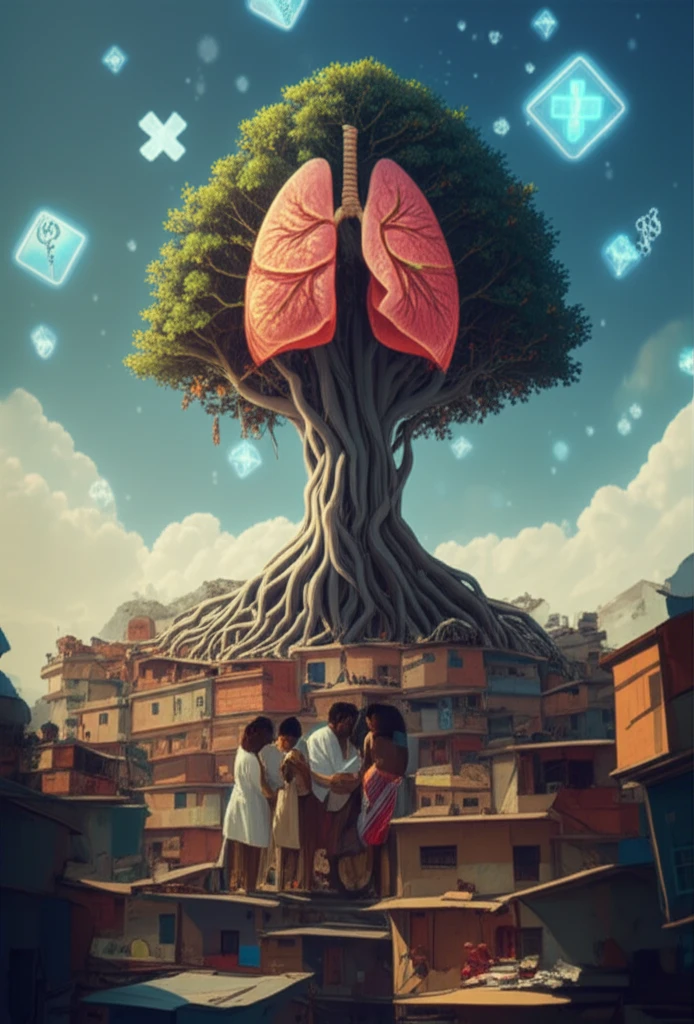
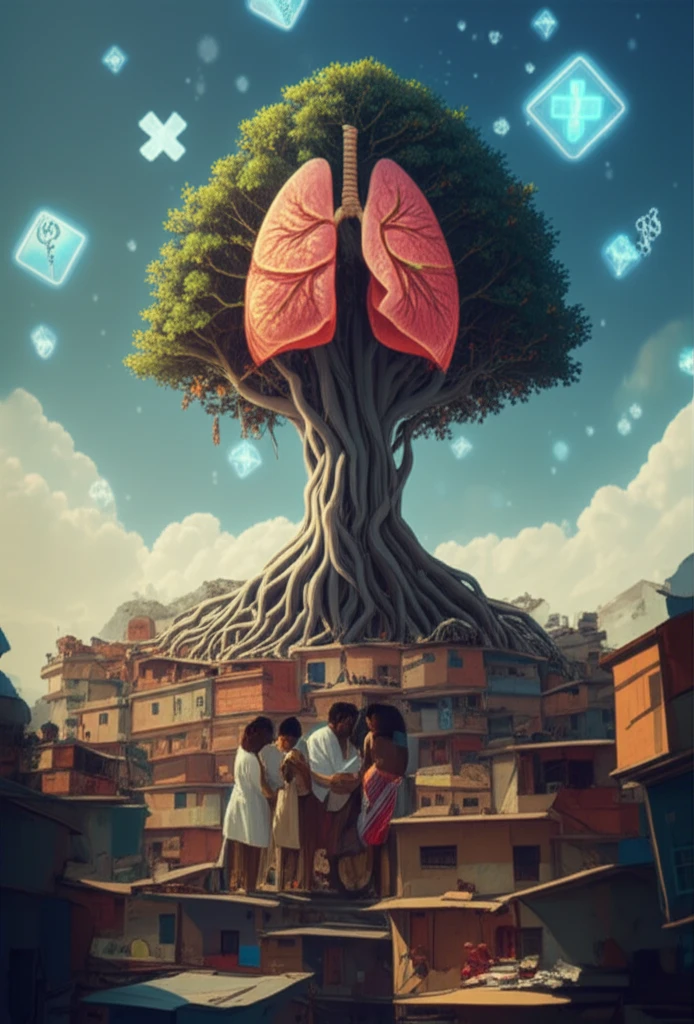
TB in Rio Grande do Sul: Unmasking Disparities and Protecting Vulnerable Communities
"A deep dive into how tuberculosis impacts indigenous populations and reveals urgent needs for tailored healthcare strategies."
Tuberculosis (TB) remains a significant public health challenge in Brazil, particularly in states like Rio Grande do Sul. While TB is treatable and preventable, its persistence reveals deeper issues of inequality and access to healthcare. Understanding these disparities is crucial for developing effective interventions and safeguarding vulnerable populations.
Rio Grande do Sul, located in southern Brazil, is among the regions with the highest TB incidence rates. Within this state, indigenous communities face a disproportionate burden of the disease, reflecting broader health inequities and systemic challenges. Addressing TB in these communities requires a focused approach that considers their unique social, cultural, and economic contexts.
A recent study analyzing data from 2003 to 2012 sheds light on the epidemiological situation of TB in Rio Grande do Sul, with a specific focus on indigenous populations. By examining trends in TB cases, treatment outcomes, and healthcare access, the research reveals critical insights for improving TB control efforts.
Unequal Impact: How TB Disproportionately Affects Indigenous Communities
The study highlights significant disparities in TB incidence rates among different racial and ethnic groups in Rio Grande do Sul. While Afro-Brazilians and indigenous peoples experience higher rates, the reasons behind these disparities are complex. Factors such as socioeconomic conditions, access to healthcare, and cultural practices all play a role.
- Higher Rates in Young Children: A notable proportion of TB cases in indigenous communities occur in children under 10 years old, a rate significantly higher than in other groups.
- Delayed Diagnosis: Indigenous populations often experience delays in diagnosis due to limited access to healthcare facilities and cultural barriers.
- Incomplete Treatment: Lower cure rates among indigenous, brown, and Afro-Brazilian populations point to challenges in treatment adherence and follow-up care.
Moving Forward: A Call for Action
The findings of this study underscore the urgent need for improved TB control efforts in Rio Grande do Sul, particularly among indigenous communities. By addressing the systemic challenges and implementing culturally sensitive interventions, we can work towards reducing disparities and protecting vulnerable populations. Further investigations are needed to deepen causes associated with the different profiles found in varied contexts.
