TAVR Complications: How to Spot and Manage This Rare Aortic Injury
"Aortic injury following Transcatheter Aortic Valve Replacement (TAVR) is rare but serious. Learn about a unique case and how a 'watch-and-wait' approach can be effective."
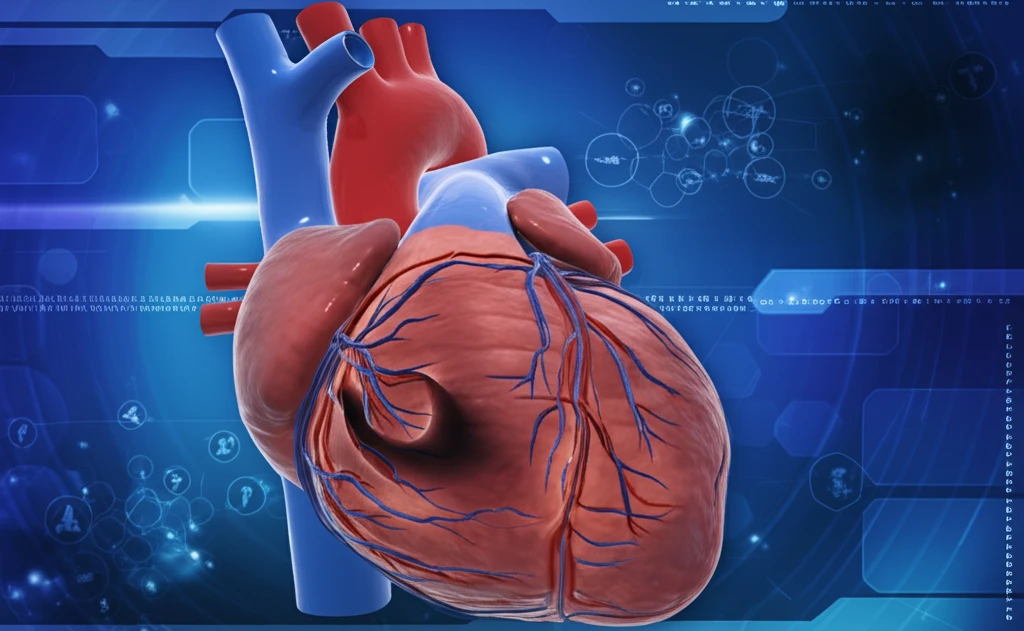
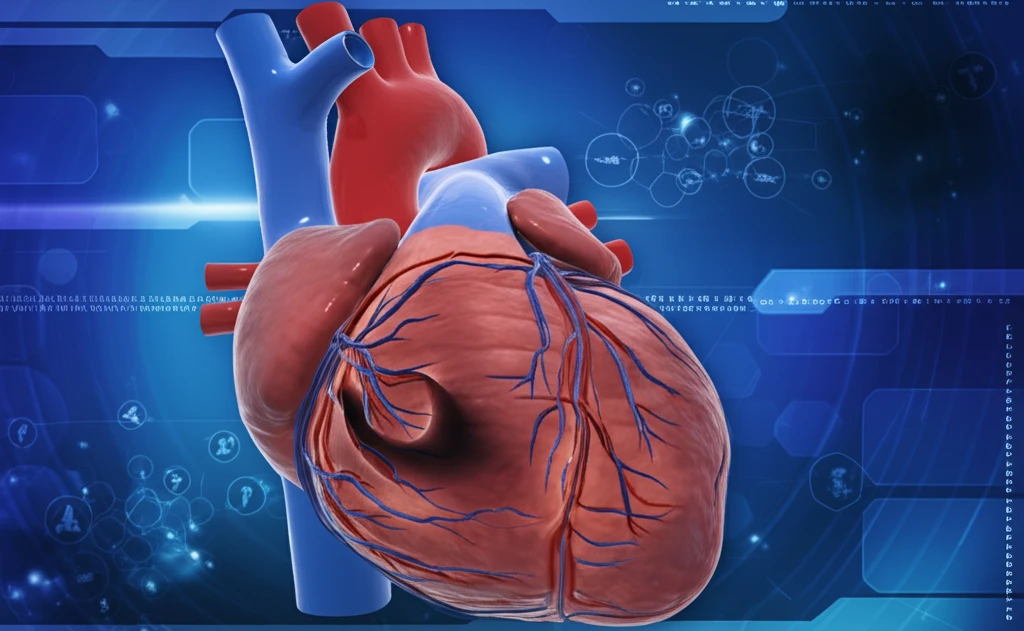
Transcatheter Aortic Valve Replacement (TAVR) has become a game-changer for individuals with severe aortic stenosis, offering a less invasive alternative to traditional surgery. While TAVR is generally safe, like all medical procedures, it carries potential risks. One such risk, though uncommon, is aortic injury.
Aortic injuries following TAVR can manifest in different ways, including aortic dissection or intramural hematoma (IMH). An intramural hematoma is characterized by bleeding within the wall of the aorta, the body's largest artery. Recognizing and managing these complications promptly and effectively is crucial for ensuring the best possible outcomes for patients.
This article delves into a fascinating case of a transient aortic intramural hematoma that occurred shortly after a TAVR procedure. We'll explore how doctors identified the issue, the treatment strategy they employed, and the remarkable recovery of the patient. This case highlights the importance of vigilance and tailored management approaches in the world of cardiac care.
Understanding Aortic Intramural Hematoma (IMH) After TAVR
In a medical study published in 'AORTA' December 2016, a case report detailed an 83-year-old woman with severe symptomatic aortic stenosis. She underwent TAVR due to her high surgical risk, indicated by a Society of Thoracic Surgeons score of 4.6 and a combined morbidity/mortality risk of 20.1%.
- Initial Presentation: 83-year-old woman with severe aortic stenosis.
- Procedure: Transcatheter Aortic Valve Replacement (TAVR).
- Complication: Development of aortic intramural hematoma (IMH) detected post-TAVR.
- Management: Conservative approach with blood pressure control and surveillance.
- Outcome: Rapid resolution of IMH observed through follow-up imaging.
The "Watch-and-Wait" Approach: Is It Right for Everyone?
The case highlights that while aortic injuries post-TAVR can be alarming, a conservative 'watch-and-wait' approach, coupled with blood pressure management and careful monitoring, can be a viable option in certain situations. This strategy is particularly relevant for elderly patients with specific criteria, like an aortic size less than 5 cm and IMH less than 11 mm. Of course, the optimal approach depends on individual patient factors, and surgical intervention remains the standard of care for acute aortic dissections post-TAVR in appropriate surgical candidates. If the dissection extends into the sinuses of Valsalva or if the coronary arteries are involved, then surgery is clearly indicated. Always consult your physician for medical advice.
