TAVI Access: Does the Route Really Matter?
"A single-center study sheds light on whether transfemoral or transapical access impacts mortality in TAVI procedures."
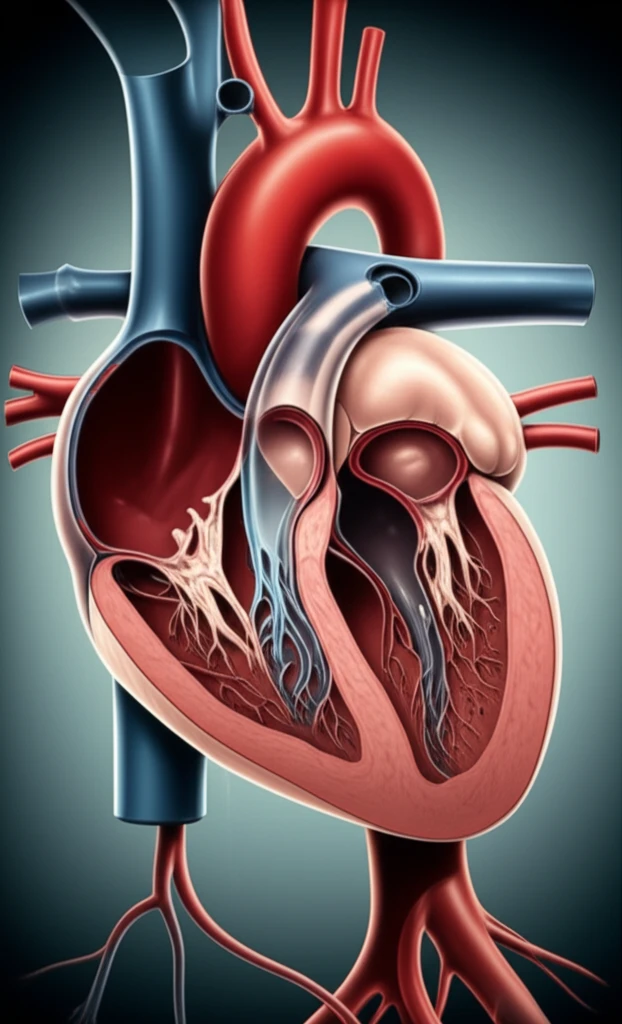
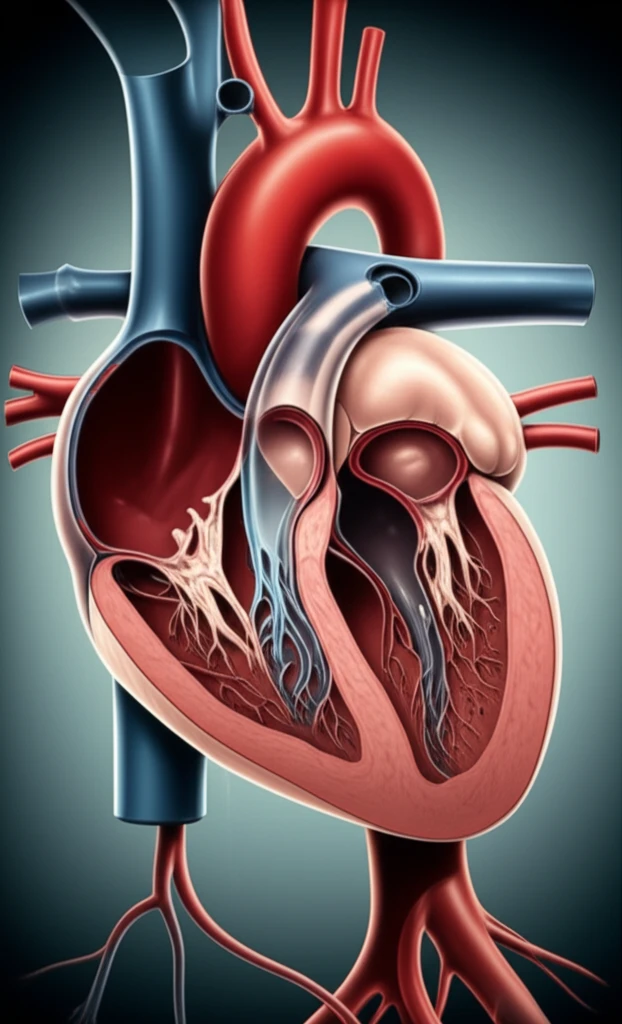
Transcatheter aortic valve implantation (TAVI) has revolutionized the treatment of severe aortic stenosis, offering a less invasive alternative to traditional open-heart surgery for high-risk patients. While TAVI's benefits are clear, debates persist regarding the optimal access route—transfemoral (TF) or transapical (TA).
The transfemoral approach, accessing the heart through the femoral artery in the leg, is often preferred due to its minimally invasive nature. However, when TF isn't feasible, the transapical approach, which involves a small incision in the chest to access the heart directly, becomes necessary. Some studies have suggested that TA-TAVI is associated with higher mortality rates compared to TF-TAVI, raising concerns about whether the access route itself contributes to increased risk.
This article explores a recent single-center study that investigated the impact of access route on TAVI outcomes. By analyzing data from 1130 patients, researchers aimed to determine whether the increased mortality observed after TA-TAVI is truly caused by the access mode or if it reflects the higher-risk profile of patients undergoing this approach. This analysis helps to clarify the factors influencing TAVI success and guides clinical decision-making.
TAVI Access: Unpacking the Research
The study, conducted at a single center, reviewed data from 1130 patients undergoing TAVI between 2009 and 2016. Of these, 619 patients underwent TF-TAVI, while 511 received TA-TAVI. Researchers meticulously compared 30-day mortality and major morbidity rates between the two groups, using the Valve Academic Research Consortium 2 (VARC-2) criteria to ensure standardized assessment.
- Unadjusted 30-day mortality was higher in TA-TAVI patients, but this difference wasn't statistically significant.
- Multivariate analysis revealed that the logistic EuroSCORE and institutional experience were independent predictors of 30-day mortality, while the access mode was not.
- Major access-site complications occurred at similar rates in both groups.
- After adjusting for risk factors, long-term mortality rates were also similar between TF-TAVI and TA-TAVI patients.
The Bigger Picture: Patient Risk vs. Access Route
This study reinforces the importance of considering patient-specific risk factors when evaluating TAVI outcomes. While the transapical approach may be necessary for certain patients, it's crucial to recognize that these individuals often have more complex medical histories.
The study also highlights the impact of institutional experience on TAVI success. As medical centers perform more TAVI procedures, their teams become more skilled at patient selection, procedural techniques, and complication management, leading to improved outcomes regardless of the access route.
Ultimately, the choice between transfemoral and transapical TAVI should be based on a comprehensive assessment of the patient's individual needs and anatomical considerations, with careful attention to risk mitigation and optimization of procedural expertise. By focusing on these factors, healthcare professionals can ensure the best possible outcomes for all TAVI patients.
