Targeting the Heart's Tricky Spots: Can New Imaging Tech Improve Ethanol Ablation for Ventricular Tachycardia?
"A new study explores how pre-procedure imaging techniques can improve the precision and effectiveness of transcoronary ethanol ablation (TCEA) for ventricular tachycardia."
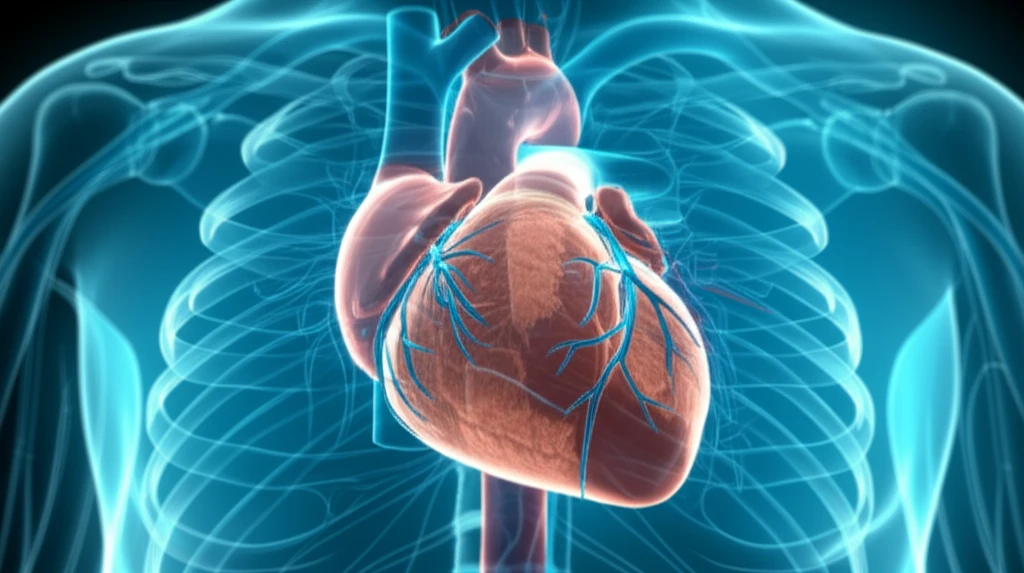
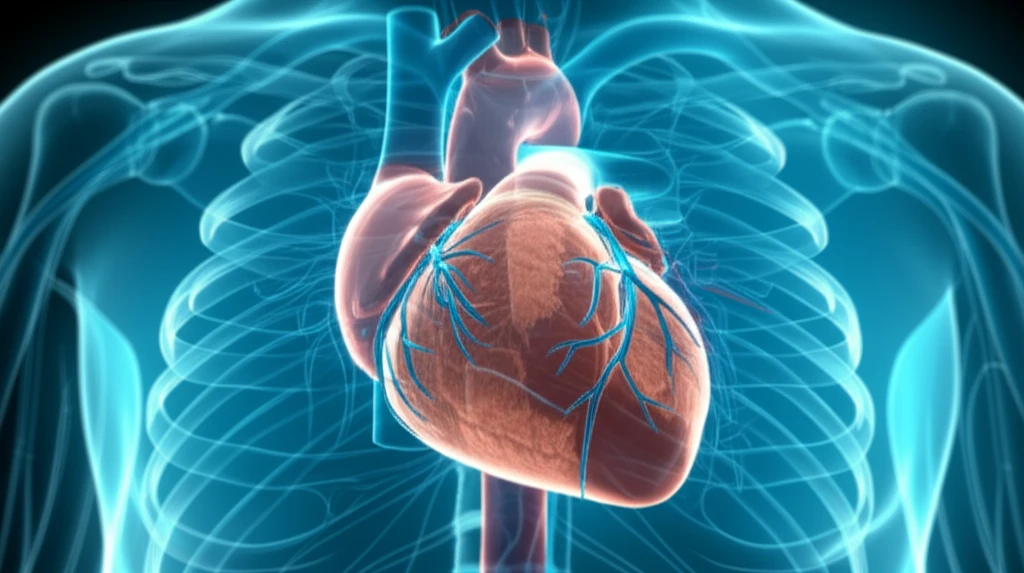
Ventricular tachycardia (VT), a rapid and erratic heartbeat originating in the heart's ventricles, can be life-threatening. Radiofrequency ablation, a common procedure to treat VT, isn't always successful, especially when the source of the arrhythmia lies deep within the heart muscle – a condition known as intramural VT. These deeply seated foci are hard to reach and eliminate with conventional methods, leading to recurrence and the need for repeated interventions.
When standard ablation fails, doctors sometimes turn to transcoronary ethanol ablation (TCEA). This involves injecting ethanol, a type of alcohol, into small coronary arteries that feed the problematic area of the heart, creating a targeted lesion to disrupt the abnormal electrical pathways. However, accurately targeting these arteries is crucial for the procedure's success and to avoid complications.
A recent study published investigates whether using detailed pre-procedural imaging can improve the precision and outcomes of TCEA for refractory septal ventricular tachycardia. The research explores how cardiac magnetic resonance (CMR) and computed tomography (CT) scans can guide the way, offering a potential solution for patients with challenging VT.
Imaging to the Rescue: How Detailed Scans Are Changing the Game
The key innovation explored in this study is the use of advanced imaging techniques before the TCEA procedure. Researchers utilized cardiac magnetic resonance (CMR) and computed tomography (CT) scans to map the heart's structure, identify the precise location of the intramural VT source, and visualize the network of coronary arteries in relation to this source. This detailed roadmap allows doctors to plan the TCEA procedure with much greater accuracy.
- Mapping the Scar: CMR was used to identify and characterize the scar tissue within the heart muscle, pinpointing the exact location of the arrhythmia's origin.
- Visualizing the Arteries: CT scans provided a detailed view of the coronary arteries, allowing doctors to select the specific septal perforator branches that supplied blood to the targeted scar tissue.
- Creating a 3D Roadmap: The CMR and CT images were merged to create a three-dimensional model of the heart, showing the relationship between the scar tissue and the coronary arteries. This roadmap was then integrated into the electroanatomical mapping system used during the TCEA procedure.
The Promising Results and Future Directions
The study found that using pre-procedural imaging to guide TCEA led to a significant reduction in VT burden for the patients. The number of ICD therapies (shocks and anti-tachycardia pacing) needed to manage their arrhythmias decreased after the procedure. This suggests that the more targeted approach, thanks to the detailed imaging, can improve the effectiveness of TCEA.
While these results are promising, the researchers emphasize that this is a small, single-center study, so larger investigations are needed to confirm these findings. However, the study provides a strong rationale for using pre-procedural imaging to guide TCEA in carefully selected patients with refractory septal VT.
This approach offers a potential way to improve outcomes for patients with challenging VT, providing a more precise and effective way to target the source of their arrhythmias. As technology advances and imaging techniques become even more sophisticated, we can expect further refinements in this approach, potentially leading to even better outcomes for patients with this difficult condition.
