Sural Flap Anatomy: A Guide to Reliable Reconstruction
"Understanding the anatomical variations of the distally based sural flap for improved surgical outcomes."
Reconstructing soft tissue defects in the distal lower leg and foot presents a significant challenge due to limited local tissue availability and the complexities of the region. Free flaps, while an option, can be complex and carry potential drawbacks.
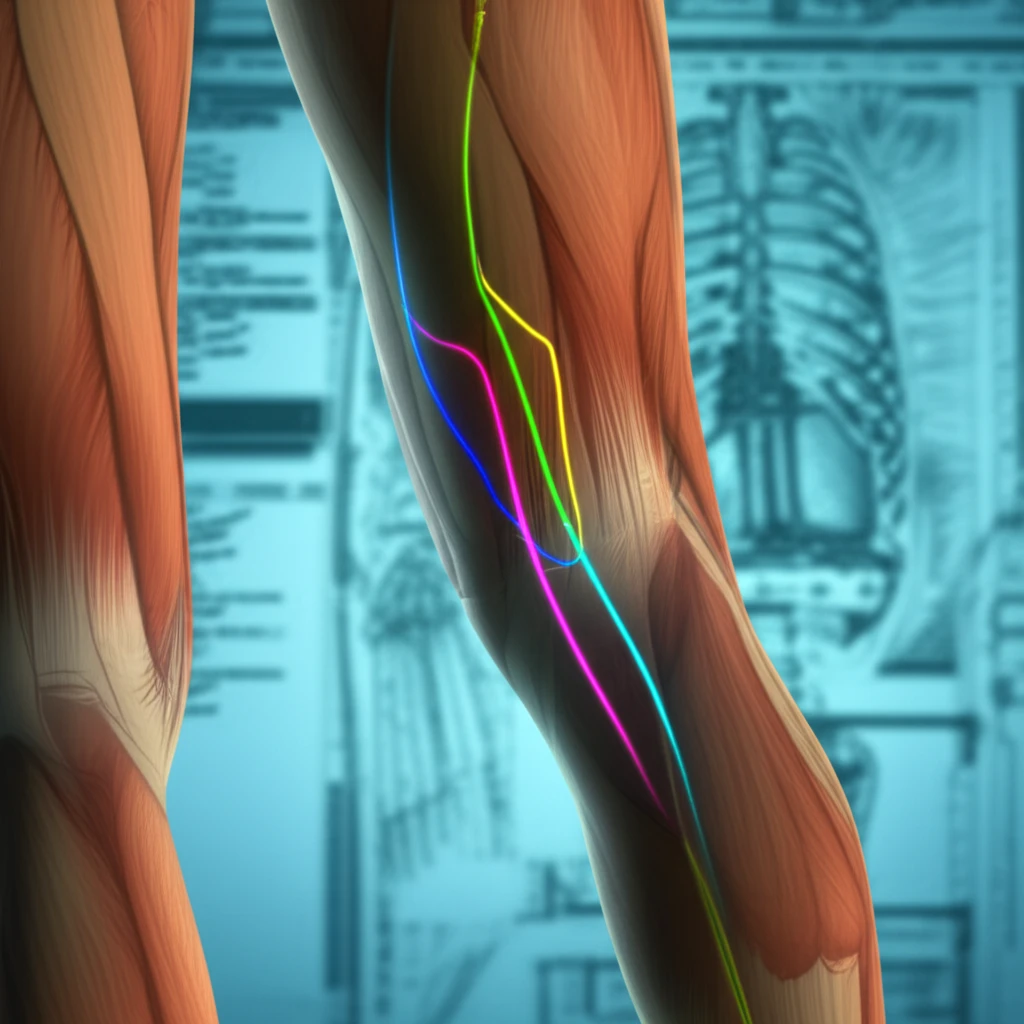
The distally based sural flap has emerged as a workhorse in reconstructive surgery for this area, offering a reliable solution for covering deep tissue defects. This fasciocutaneous flap relies on the sural artery and its perforators, making a thorough understanding of its anatomy crucial for successful outcomes.
This article delves into the anatomical intricacies of the sural flap, drawing upon cadaveric studies to provide surgeons with a detailed understanding of the flap's vascular supply and potential variations. By exploring these anatomical nuances, we aim to equip surgeons with the knowledge to optimize flap design and minimize complications.
Unveiling the Sural Flap's Blood Supply: Key Anatomical Insights
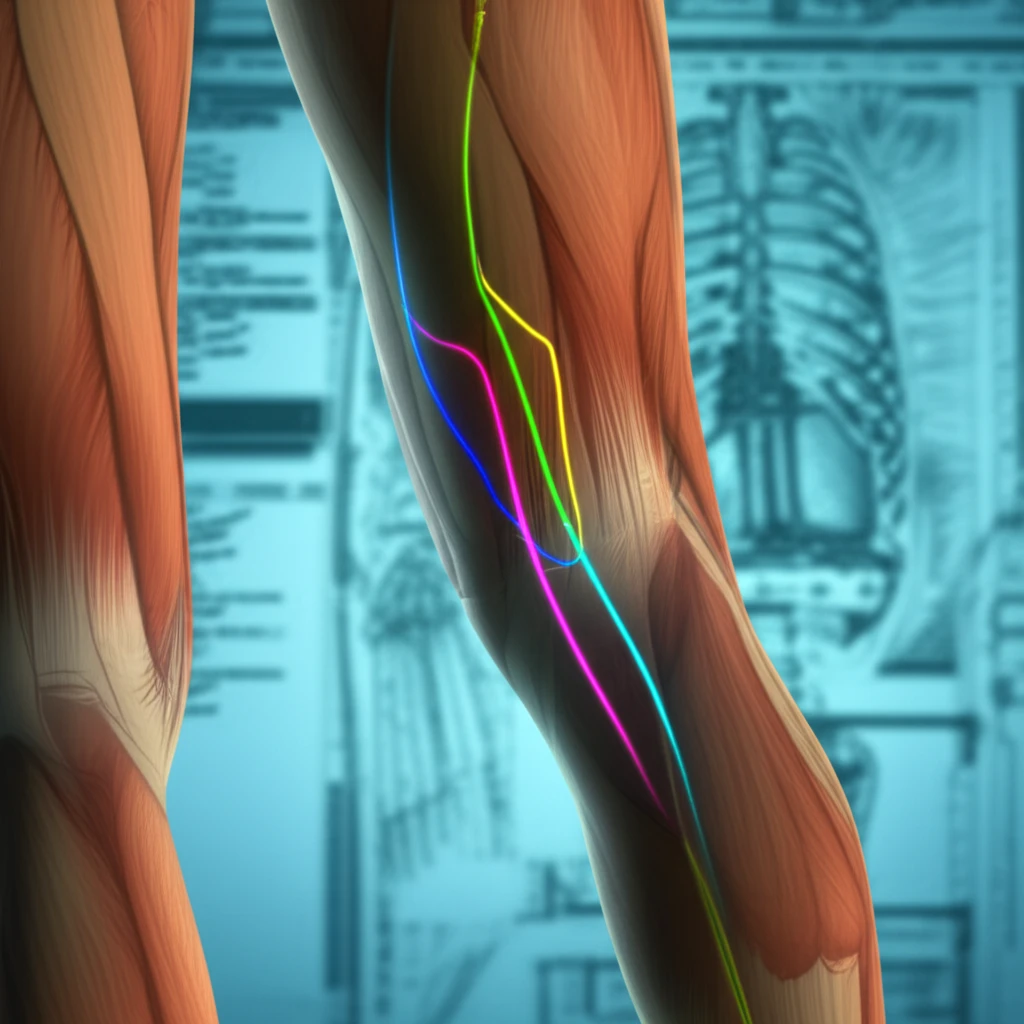
A cadaveric study was conducted on eight lower limbs to meticulously map the arterial supply of the distally based sural flap. Red latex was injected into the popliteal artery, followed by careful dissection to reveal the fasciomyocutaneous flap and its vascular pedicle. The focus was on identifying and measuring the perforating arteries originating from the sural artery.
- Sural Nerve as a Guide: The sural nerve was consistently identified in all dissections, serving as a reliable landmark for locating the vascular pedicle.
- Perineural Plexus Dominance: In a significant number of cases, the primary blood supply to the flap originated from a perineural plexus surrounding the sural nerve.
- Arterial Variations: The study observed variations in the sural artery's presentation, including the presence of three distinct sural arteries (lateral, median, and medial) in some dissections, while others exhibited only lateral or combined lateral and medial arteries.
- Perforator Distribution: The number of perforating arteries varied, with 3 to 6 perforators identified on the medial side of the pedicle and 4 to 5 on the lateral side.
Optimizing Sural Flap Design: Key Takeaways for Surgeons
The study's findings emphasize the variable nature of the sural artery's distribution, with the perineural plexus being a common source of blood supply. This suggests that flap design should prioritize the inclusion of the sural nerve and its surrounding tissue to maximize vascularity.
Based on the perforator mapping, the pivot point of the flap—the point around which the flap is rotated—should be approximately 5.5 cm above the lateral malleolus. This positioning optimizes the inclusion of key perforating arteries in the flap's pedicle.
By carefully considering these anatomical factors and adapting surgical techniques accordingly, surgeons can enhance the reliability and success of distally based sural flaps in lower limb reconstruction.
