Stroke Treatment Showdown: Thrombolysis First or Straight to Endovascular?
"Decoding the best strategy for acute stroke: When does dissolving the clot upfront make a difference?"
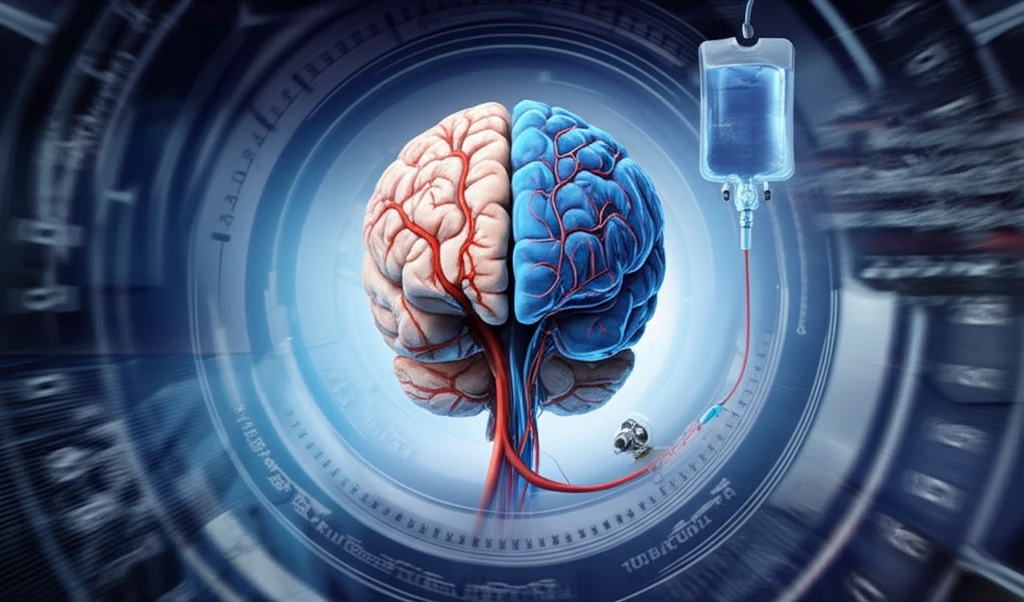
In the fast-paced world of stroke treatment, time is brain. Every minute counts when a blood clot blocks an artery, starving brain tissue of oxygen and nutrients. For years, the standard approach for acute ischemic stroke—the most common type—has been intravenous thrombolysis (IVT), using a drug like alteplase (tPA) to dissolve the clot. However, the rise of endovascular treatment (EVT), a minimally invasive procedure to physically remove the clot, has sparked a crucial debate: Should we always thrombolyse first, or should some patients go straight to endovascular intervention?
This question isn't just academic; it has profound implications for patient outcomes. Stroke protocols vary worldwide, and knowing when to prioritize one treatment over the other—or combine them—can significantly impact a person's chances of recovery. While endovascular treatment has proven highly effective for large vessel occlusions (LVOs), where major arteries are blocked, the role of upfront thrombolysis remains a topic of intense investigation. Many patients receive both treatments, but is this always necessary, and does it truly improve results?
This article delves into the heart of this controversy, analyzing the latest research and expert opinions to shed light on the optimal strategy for acute stroke management. We'll explore the benefits and drawbacks of each approach, examine the evidence for combined therapy, and consider the factors that guide treatment decisions in the real world. By understanding the nuances of this debate, we can empower ourselves to make informed choices about stroke care and advocate for the best possible outcomes.
Thrombolysis (IVT): The Traditional First Line of Defense
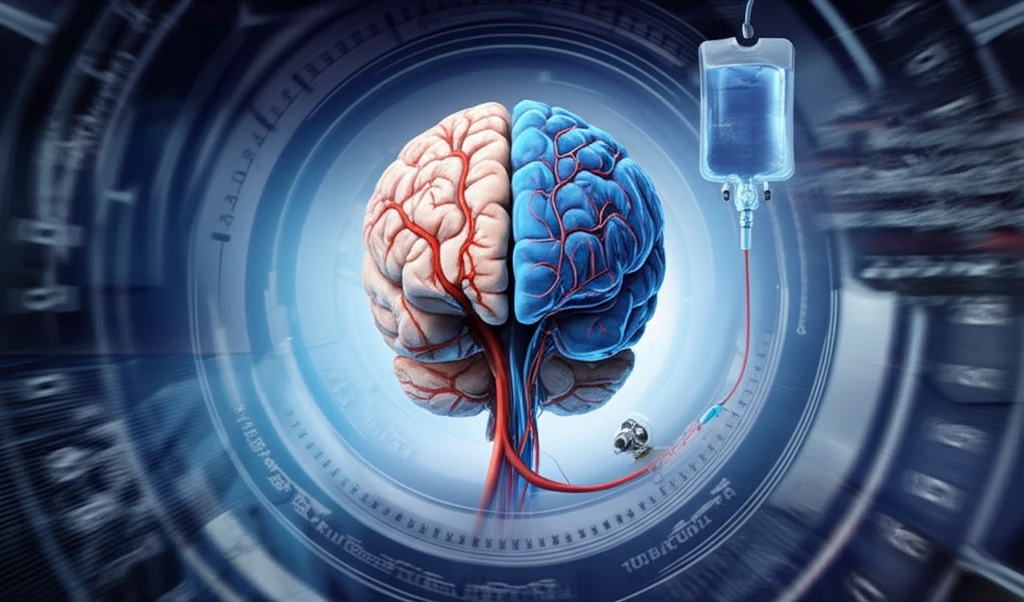
For decades, intravenous thrombolysis has been the cornerstone of acute stroke treatment. Administered through a vein, tPA works by activating plasminogen, a protein in the blood that helps dissolve clots. The sooner tPA is given, the better the chance of restoring blood flow and minimizing brain damage. Landmark trials have established the effectiveness of IVT within a specific time window (typically 4.5 hours from symptom onset), making it a widely accessible treatment option.
- Limited Effectiveness for Large Clots: tPA may not be powerful enough to fully dissolve large vessel occlusions, leaving significant areas of the brain at risk.
- Bleeding Risk: Thrombolysis carries a risk of bleeding, including intracranial hemorrhage (ICH), a serious complication that can worsen outcomes.
- Time Sensitivity: The benefits of tPA diminish rapidly with time, emphasizing the need for rapid diagnosis and treatment.
The Road Ahead: Optimizing Stroke Treatment Strategies
The debate over thrombolysis versus endovascular therapy is far from settled. Ongoing research continues to refine our understanding of the optimal approach for different patient profiles. As technology advances and treatment strategies evolve, the future of stroke care promises even more effective ways to minimize brain damage and improve patient outcomes. By staying informed and advocating for evidence-based practices, we can all play a part in transforming the landscape of stroke treatment.
