Stent Success: Can Blood Speckle Predict Long-Term Artery Health?
"New research explores how intraluminal blood speckle intensity (AIBS) measurements during intravascular ultrasound (IVUS) can predict the long-term success of coronary stent implants and reduce the need for repeat procedures."
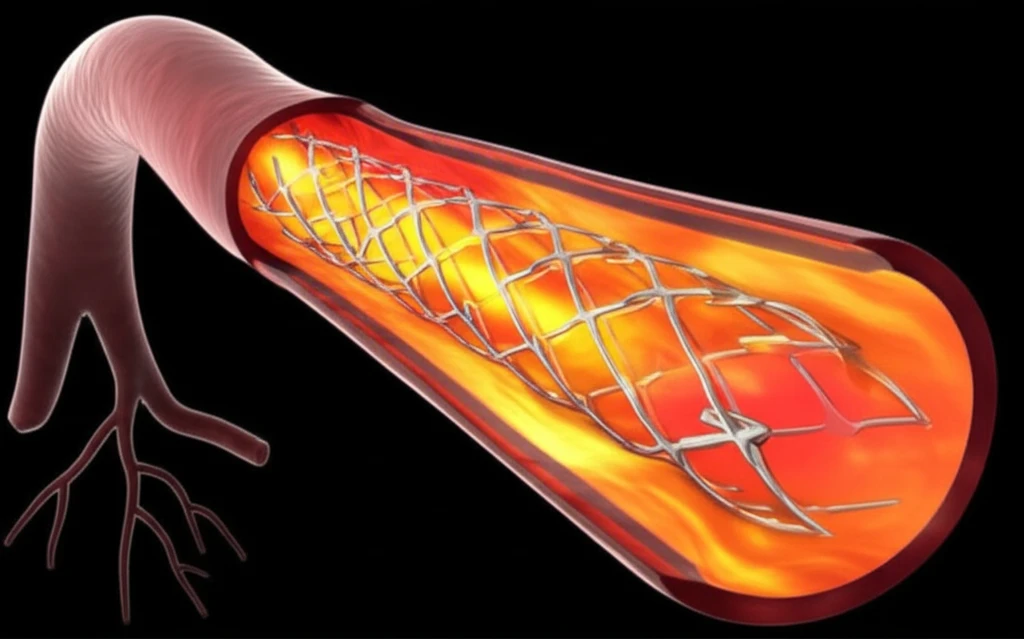
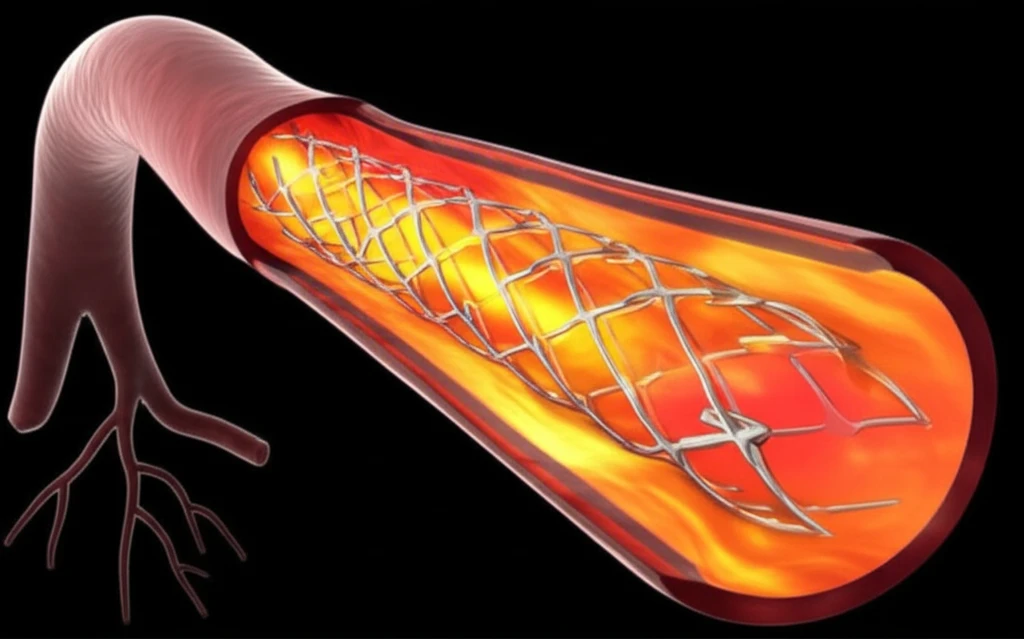
Coronary artery disease, a condition characterized by the buildup of plaque inside the coronary arteries, is a leading cause of heart-related issues globally. Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a procedure used to open up these blocked arteries, often involving the placement of a stent to keep the artery open. While drug-eluting stents (DES) have greatly reduced the risk of arteries re-narrowing compared to bare-metal stents, a significant number of patients still require repeat procedures, known as target vessel revascularization (TVR).
Fractional flow reserve (FFR) is a technique used to assess the physiological severity of coronary artery narrowings and is considered the gold standard in deciding whether to proceed with interventions like stenting. Optimizing PCI with FFR guidance has been shown to improve patient outcomes. However, intravascular ultrasound (IVUS) offers another valuable approach to optimizing PCI, with studies suggesting that IVUS-guided PCI can decrease the need for revascularization compared to relying solely on angiography. While minimal stent area (MSA) as assessed by IVUS is a known predictor of in-stent restenosis, its predictive power is limited to target lesion revascularization (TLR) and is heavily dependent on vessel size.
Recent research has focused on a new parameter measurable via IVUS: the difference in intraluminal intensity of blood speckle (IBS), termed AIBS (ΔΙBS), across a coronary artery stenosis. This measurement, obtained using integrated backscatter (IB)-IVUS, has shown promise in correlating with FFR values. The critical question, however, is whether AIBS measurements taken post-PCI can predict the need for future TVR. A new study has sought to explore this potential link, offering hope for more accurate prediction of long-term stent success.
How Can AIBS Measurements Improve Stent Outcomes?
The study, conducted at Chiba University Hospital, screened 703 vessels that underwent PCI with stents between April 2013 and December 2014. After excluding vessels based on specific criteria such as lack of IVUS guidance or follow-up information, 393 vessels in 298 patients were included in the final analysis. Follow-up coronary angiography (CAG) was routinely performed about 12 months post-PCI. The primary endpoint was TVR, defined as any clinically driven repeat intervention from the ostium to 5 mm distal to the implanted stent in the target vessel.
- AIBS as a Predictor: The study found that AIBS was significantly greater in vessels that required TVR compared to those that did not (11.10 ± 5.93 vs. 5.90 ± 5.49, P <0.001).
- ROC Curve Analysis: Receiver operating characteristic (ROC) curve analysis showed that AIBS significantly predicted TVR (AUC 0.74, best cut-off value 8.24, P < 0.001).
- Independent Predictors: Multiple logistic regression analysis identified the use of drug-eluting stents and AIBS values above 8.24 as independent predictors of TVR.
Future Implications
This research opens new avenues for improving long-term outcomes in patients undergoing PCI. By incorporating AIBS measurements into routine IVUS assessments, clinicians may be able to better predict which patients are more likely to experience TVR. This could lead to tailored intervention strategies, such as more aggressive post-dilation or the use of specific stent types, to optimize outcomes and reduce the need for repeat procedures. Further studies are needed to validate these findings and explore the optimal methods for incorporating AIBS into clinical practice.
