Stent Graft Infections: Understanding the Risks, Symptoms, and Treatments
"A comprehensive guide to recognizing, managing, and preventing infections associated with endovascular stent grafts."
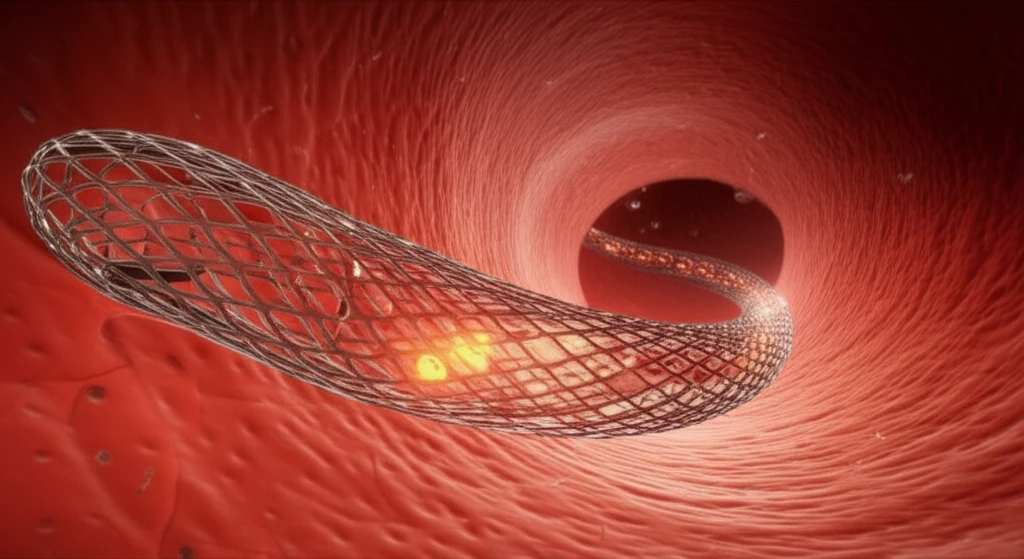
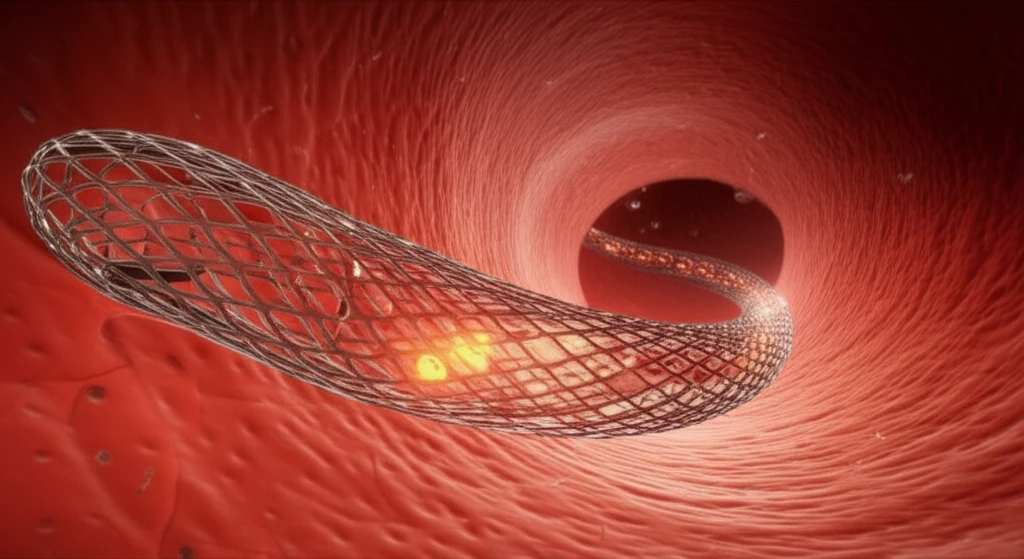
Endovascular stent grafts have revolutionized the treatment of vascular diseases, offering a minimally invasive alternative to traditional open surgery. These devices, typically used to repair aneurysms or blockages in blood vessels, provide structural support and redirect blood flow. While generally safe, a potential complication is infection, which, though infrequent, can lead to significant health risks.
Infections involving stent grafts are particularly concerning due to their association with high mortality rates. Early detection and appropriate management are crucial to improving patient outcomes. This article aims to provide a comprehensive overview of stent graft infections, covering aspects from risk factors and clinical presentation to diagnosis and treatment strategies.
By understanding the nuances of stent graft infections, patients and healthcare providers can work together to minimize risks and ensure the best possible care. We'll explore the latest research and clinical guidelines to equip you with the knowledge needed to navigate this challenging condition.
What are the Risk Factors for Stent Graft Infections?
Several factors can increase the risk of developing a stent graft infection. Unlike traditional open surgeries, endovascular procedures are often performed percutaneously, leading to the initial perception that infections would be rare. However, the expanding use of endovascular techniques and the increasing frequency of stent graft placements have highlighted infectious complications as a noteworthy concern.
- Immunosuppression: Patients with weakened immune systems are more susceptible to infections.
- Location of Procedure: The site of the endovascular procedure can influence infection risk.
- Treatment of Pseudoaneurysms and Mycotic Aneurysms: Procedures addressing these conditions carry an elevated risk.
- Presence of Neoplasia: Individuals with cancer may have compromised immune defenses.
- Corticosteroid Use: Long-term use of corticosteroids can suppress the immune system.
The Future of Stent Graft Infection Management
Stent graft infections, while infrequent, represent a significant challenge in vascular surgery. Prompt investigation and aggressive treatment are essential to improve outcomes. The approach mirrors that of traditional surgical infections, emphasizing complete excision of the infected graft and revascularization, either in situ or via extra-anatomical bypass. Conservative management is reserved for select high-risk patients with early-stage infections and no complications.
