Stent Failure in Ureteral Obstruction: Are You at Risk?
"A new risk stratification model helps predict ureteral stent failure, allowing for personalized treatment plans and better patient outcomes."
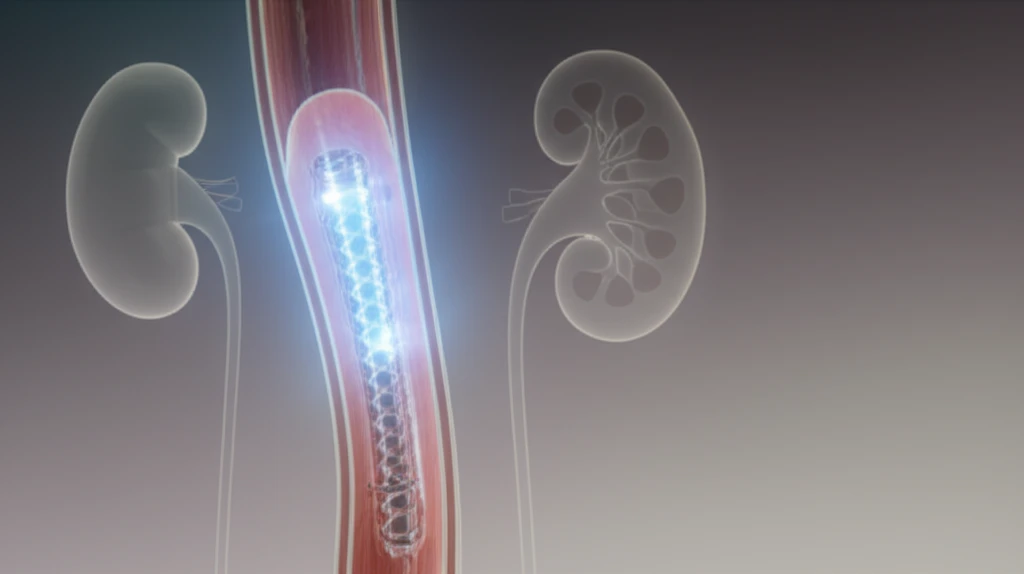
Malignant extrinsic ureteral obstruction (MUO) occurs when a tumor or growth outside the ureter (the tube that carries urine from the kidney to the bladder) presses on it, blocking the flow of urine. This can lead to serious complications, including kidney damage and even death. Ureteral stents are frequently used to open up the blockage, providing relief and maintaining kidney function. However, these stents can fail, requiring additional procedures and impacting a patient's quality of life. If untreated, ureteral obstruction can lead to renal failure and even death [4]. However, there is evidence that palliative urinary diversion prevents the deterioration of renal failure and may result in improved survival [5].
The challenge lies in predicting which patients are most likely to experience stent failure. Recognizing risk factors early on allows doctors to make more informed decisions about initial treatment strategies, potentially avoiding unnecessary procedures and improving patient outcomes. Current methods of managing MUO often involve ureteral internal stents, percutaneous nephrostomy (PCN) catheters, or extra-anatomic stents in order to provide symptomatic relief and maintain renal function.
A recent study published in the International Journal of Clinical Oncology has shed light on this critical issue, identifying key factors that predict ureteral stent failure in patients with MUO. This article breaks down the study's findings, explaining a new risk stratification model that can help doctors better manage this challenging condition. We will also provide a detailed explanation about the article and its data points for the audience.
What Predicts Stent Failure? Key Risk Factors Identified
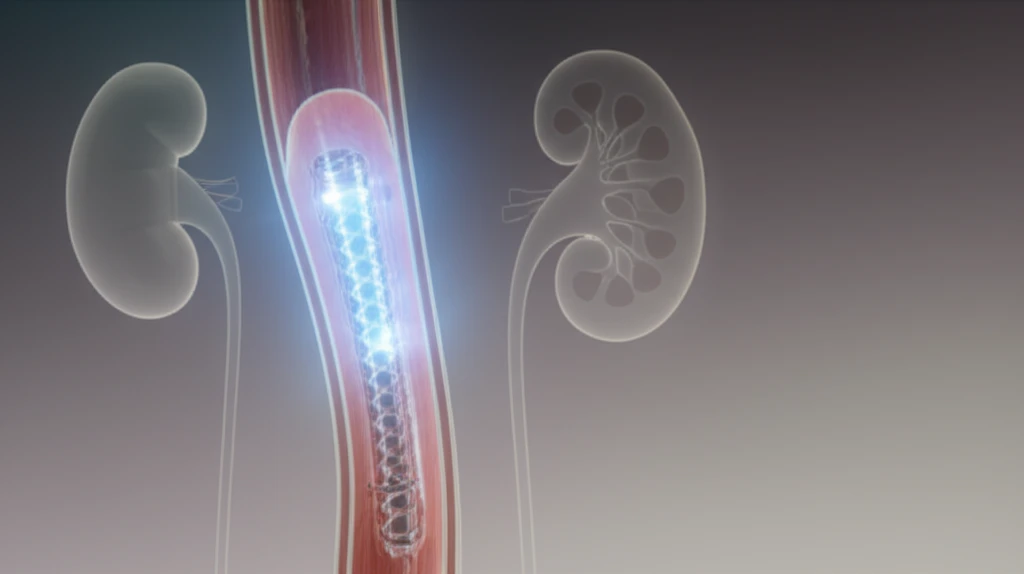
The study, led by Hiroshi Matsuura and colleagues, retrospectively analyzed data from 91 patients who underwent ureteral stent placement for MUO. The researchers looked at various clinical and radiological factors to determine which ones were associated with stent failure. Stent failure was defined as the necessity for another alternative form of urinary diversion (including PCN or an external ureteral stent) for one of the following reasons: an inability to replace the ureteral stent; increasing serum creatinine levels; complication by obstructive pyelonephritis; or the presence of a recurrent stent obstruction.
- Bladder Invasion: When the cancer has spread to involve the bladder.
- Severe Hydronephrosis: Significant swelling of the kidney due to the backup of urine before stent insertion. The severity of hydronephrosis was evaluated by US according to the grading system of the Society for Fetal Urology.
Empowering Patients and Optimizing Care
This study provides valuable insights for managing patients with malignant extrinsic ureteral obstruction. By identifying those at high risk of stent failure, clinicians can make informed decisions about initial treatment strategies, potentially improving patient outcomes and quality of life. The findings also highlight the importance of shared decision-making, ensuring that patients are fully informed about the risks and benefits of different treatment options.
