Stem Cell Breakthrough: How Tiny Vesicles Could Revolutionize Ischemia Treatment
"Extracellular vesicles from mesenchymal stem cells activate VEGF receptors, accelerating recovery from hindlimb ischemia and offering new hope for regenerative medicine."
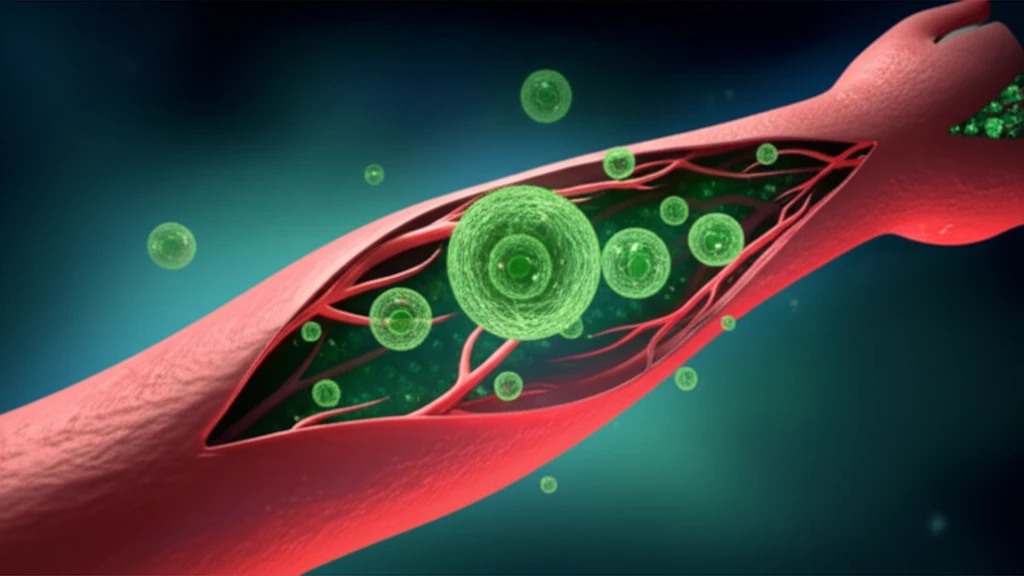
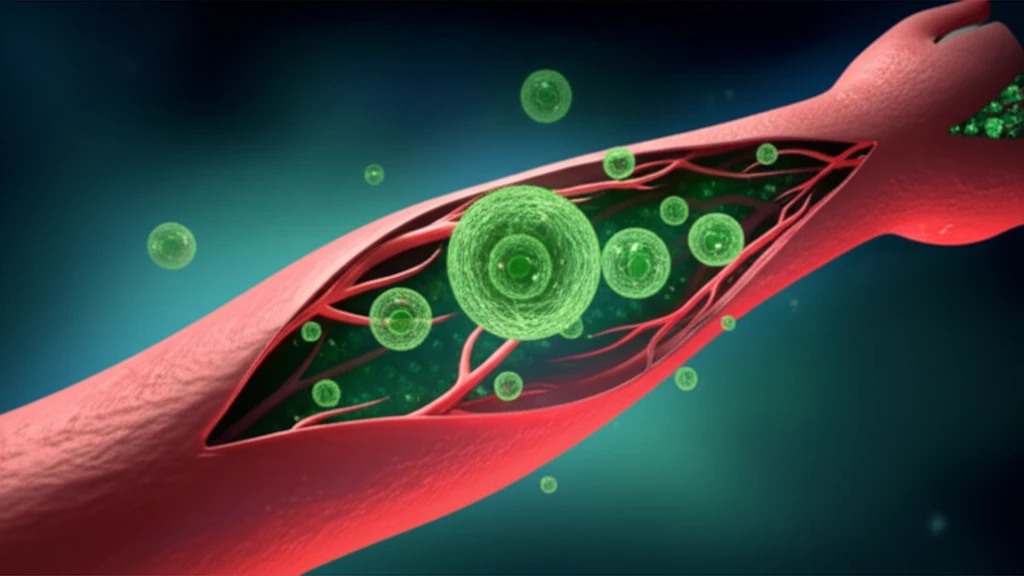
For years, scientists have explored mesenchymal stem cells (MSCs) as potential therapies for a variety of diseases. These cells, known for their ability to develop into various cell types, hold immense promise in regenerative medicine. However, the exact mechanisms behind their therapeutic efficacy, particularly in promoting angiogenesis (the formation of new blood vessels), have remained unclear. But what if the key to unlocking their potential lies in tiny vesicles they release?
New research illuminates how MSCs exert their regenerative effects, focusing on extracellular vesicles (EVs). These EVs, derived from MSCs, have shown remarkable capabilities in activating VEGF receptors and accelerating recovery from hindlimb ischemia. This breakthrough not only deepens our understanding of stem cell therapies but also opens up new avenues for treating ischemic conditions, where blood flow is restricted.
The study highlights how these MSC-derived EVs can stimulate angiogenesis, a critical process for tissue repair and recovery in ischemic diseases. By understanding the mechanisms through which EVs activate VEGF receptors, scientists are paving the way for more targeted and effective treatments. This discovery could transform how we approach regenerative medicine, offering hope for improved outcomes in various ischemic conditions.
Unlocking the Potential of MSC-EVs: Activating VEGF Receptors for Enhanced Recovery
The research team began by isolating MSC-EVs from mouse cell cultures, employing meticulous techniques such as transmission electron microscopy and nanoparticle analysis to characterize these vesicles. These methods confirmed the purity and structure of the isolated EVs, setting the stage for in vitro experiments to assess their angiogenic potential. The analysis confirmed that the MSC-EVs had a average diameter of 134.8 nm, and contained proteins ALIX and CD63, but not other proteins.
- Migration Assays: Endothelial cells were treated with MSC-EVs to observe changes in their ability to migrate, a crucial step in angiogenesis.
- Proliferation Assays: The impact of MSC-EVs on endothelial cell growth was examined, assessing whether these vesicles could stimulate cell division and expansion.
- Tube Formation Assays: Endothelial cells were cultured on a matrix gel to assess their capacity to form tube-like structures, mimicking the formation of new blood vessels.
Toward Clinical Applications: Future Directions and Therapeutic Potential
This study marks a significant step forward in understanding the therapeutic potential of MSC-EVs. By elucidating the mechanisms through which these vesicles activate VEGF receptors and promote angiogenesis, researchers are paving the way for innovative treatments for ischemic diseases. As the field progresses, future studies will likely focus on optimizing EV-based therapies for clinical use, potentially transforming the lives of individuals affected by these debilitating conditions. Ultimately, this research underscores the power of regenerative medicine and the potential of stem cell-derived therapies to revolutionize healthcare.
