Skin Moles and Keratinocytic Nevi: What You Need to Know
"A comprehensive guide to understanding epidermal nevi, their genetic origins, and associated syndromes."
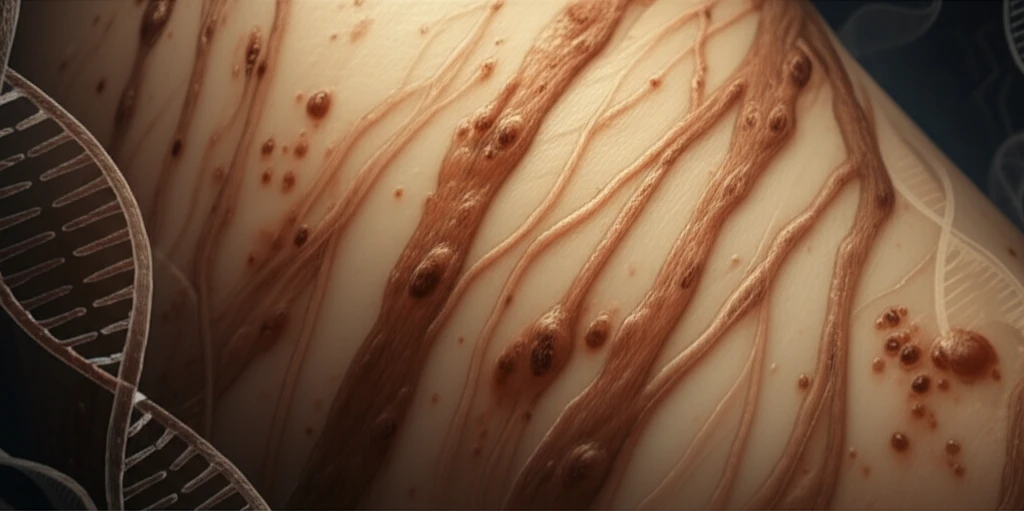
Skin moles, clinically known as nevi, are common. Epidermal nevi, specifically, are benign, tumor-like malformations that originate from the epidermis and sometimes the skin's adnexal structures (like hair follicles and sweat glands). Historically, these nevi have been categorized by their appearance. However, recent genetic research has begun to shed light on their origins and links to other health conditions.
This article dives into the world of epidermal nevi, focusing on keratinocytic nevi. We'll explore how these skin lesions develop, what genetic factors are involved, and what associated syndromes you should be aware of. This is the first part of a series, focusing specifically on nevi derived from the epidermis.
Whether you're someone with a newfound interest in skin health, have noticed a mole that concerns you, or simply want to expand your knowledge, this guide offers accessible insights into the nature, genetics, and potential implications of keratinocytic nevi.
What are Keratinocytic Nevi and How Do They Develop?
A hamartoma, the origin of skin nevi, is a benign, tumor-like malformation that arises due to an abnormal mixture of mature tissue elements. Unlike neoplasms, hamartomas don't involve autonomous, uncontrolled growth. When these occur in the skin, they're called nevi.
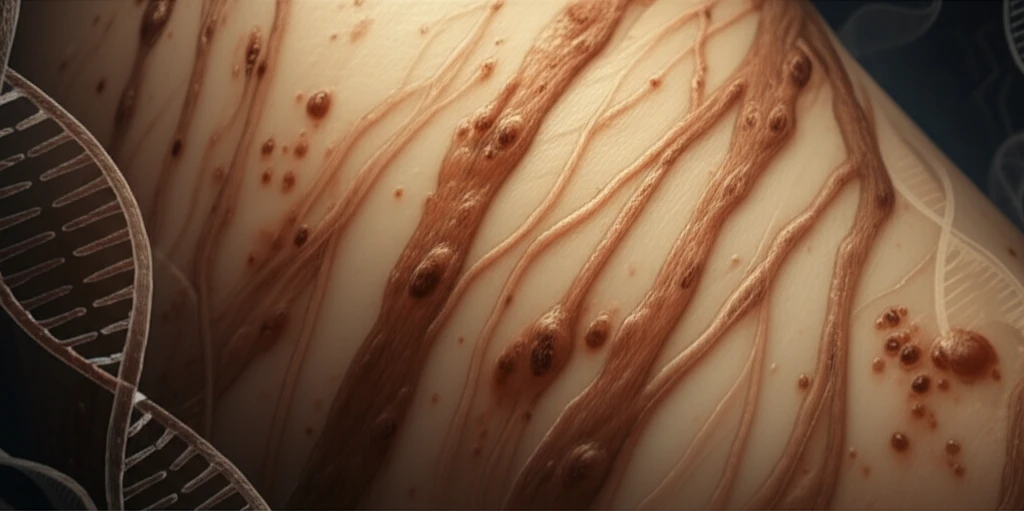
- Somatic mutations in autosomal dominant genes: These mutations, which would be lethal in a zygote, persist in a mosaic form, affecting only a group of cells that survive due to proximity to normal cells. These mutations often involve the PI3K and MAP-kinase pathways, crucial for cell survival and proliferation.
- Nonlethal mutations in autosomal genes: These mutations cause extensive skin disease when present in the zygote but can manifest in mosaic form following a postzygotic mutation. This can lead to exclusively mosaic involvement in otherwise healthy individuals (type 1 Happle mosaicism) or occur in patients already presenting a generalized form of the disease (type 2 mosaicism).
- Mosaic mutations or epigenetic changes: These occur in genes linked to polygenic inflammatory diseases.
- Functional mosaicism: This is linked to random X chromosome inactivation in women, also known as lyonization.
Key Takeaways and Next Steps in Understanding Keratinocytic Nevi
Keratinocytic nevi are complex skin lesions arising from genetic mosaicism during development. While typically benign, understanding their genetic basis and potential associations with syndromes is crucial.
If you notice a new or changing mole, particularly one that follows a linear pattern or is associated with other unusual symptoms, consult a dermatologist. Genetic testing and careful clinical evaluation can help determine the nature of the lesion and any associated risks.
This article serves as a starting point. As research progresses, our understanding of epidermal nevi and their genetic underpinnings will continue to evolve, leading to improved diagnostics and management strategies. Stay informed and proactive about your skin health.
