Silent Danger: Unmasking Retroperitoneal Hematoma Risks with Blood Thinners
"Learn how common blood thinners can sometimes lead to a serious, hidden bleeding condition and what you can do to stay safe."
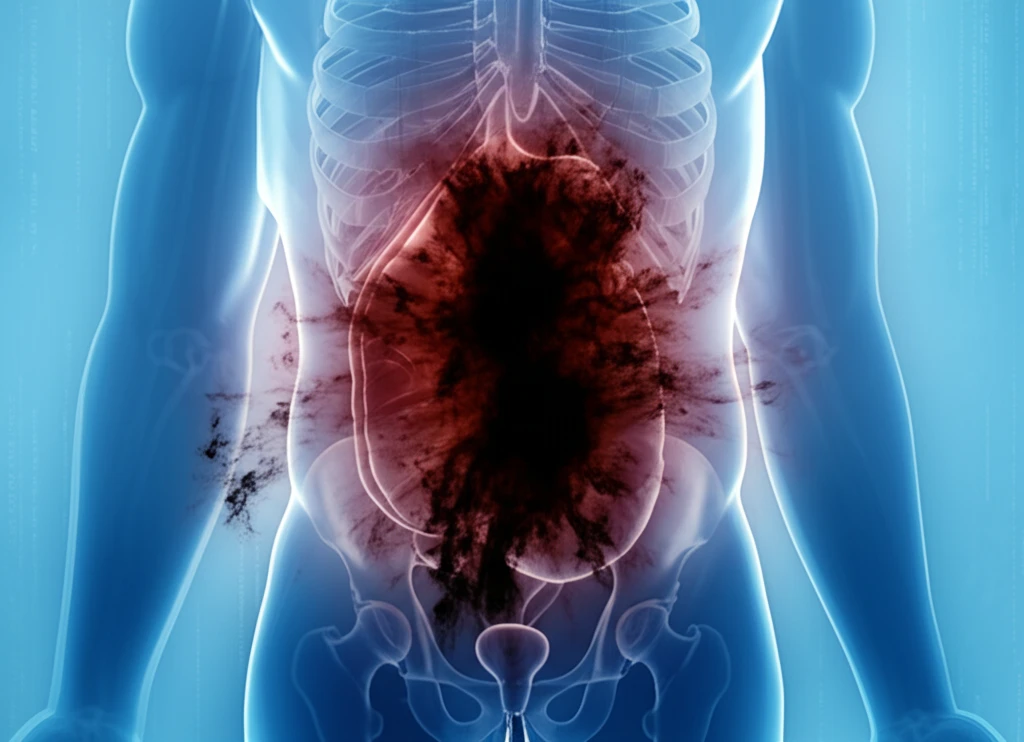
Blood thinners, also known as anticoagulants and antiplatelet drugs, are essential medications for preventing life-threatening conditions like strokes and heart attacks. However, like any medication, they come with potential risks. One of the most serious, though rare, side effects is spontaneous retroperitoneal hematoma (SRH), a condition where bleeding occurs in the retroperitoneal space—the area behind the abdominal cavity—without any trauma or surgical cause.
SRH is a medical emergency that requires prompt diagnosis and treatment. Understanding the potential risks associated with blood thinners and recognizing the symptoms of SRH can help patients and healthcare providers act quickly, improving outcomes and potentially saving lives. This article explores the characteristics, risk factors, and management strategies for SRH, providing crucial information for anyone taking or considering blood-thinning medications.
While blood thinners offer significant benefits, particularly for those at risk of blood clots, it’s important to be aware of the less common but severe complications like SRH. By staying informed and maintaining open communication with your healthcare provider, you can navigate the benefits and risks effectively.
Understanding Spontaneous Retroperitoneal Hematoma
Spontaneous retroperitoneal hematoma (SRH) is a rare condition characterized by bleeding into the retroperitoneal space. This area, located behind the abdominal cavity, houses vital organs and structures, including the kidneys, pancreas, and major blood vessels. Unlike hematomas caused by trauma or surgery, SRH occurs without any external injury or medical intervention. This makes it particularly challenging to diagnose, as the symptoms can be subtle and easily mistaken for other conditions.
- Age: Elderly patients are more susceptible due to age-related changes in blood vessels and organ function.
- Comorbidities: Conditions like hypertension, diabetes, chronic kidney disease, and cardiovascular diseases can weaken blood vessels, making them more prone to rupture.
- Polypharmacy: Taking multiple medications simultaneously increases the risk of drug interactions, potentially amplifying the effects of blood thinners.
- Kidney and Liver function: Impaired kidney or liver function can affect the metabolism and excretion of blood thinners, leading to elevated drug levels and increased bleeding risk.
Protecting Yourself: Awareness and Action
If you’re taking blood thinners, being proactive about your health is essential. Stay vigilant for any unusual symptoms and maintain regular check-ups with your healthcare provider. Discuss your medication regimen, including any over-the-counter drugs or supplements, to identify potential interactions. Inform your doctor immediately if you experience any signs of bleeding, such as unexplained bruising, nosebleeds, or blood in your urine or stool. Early detection and prompt management can significantly improve outcomes and ensure that you continue to benefit from your blood-thinning medication with minimal risk.
