Shoulder Arthroplasty: Is a 'Dry Catheter' the Key to Safer Pain Management?
"Explore how a novel technique in regional anesthesia can help distinguish surgical complications from nerve-related issues in shoulder replacement surgery."
Total shoulder arthroplasty (TSA) aims to restore movement and relieve pain for individuals with severe shoulder joint damage. Post-surgery pain control is paramount. Effective pain relief allows patients to engage in physical therapy sooner, shortens hospital stays, and boosts overall satisfaction. When pain is poorly managed, it can trigger physiological stress responses, limit mobility, and even increase the risk of deep vein thrombosis (DVT).
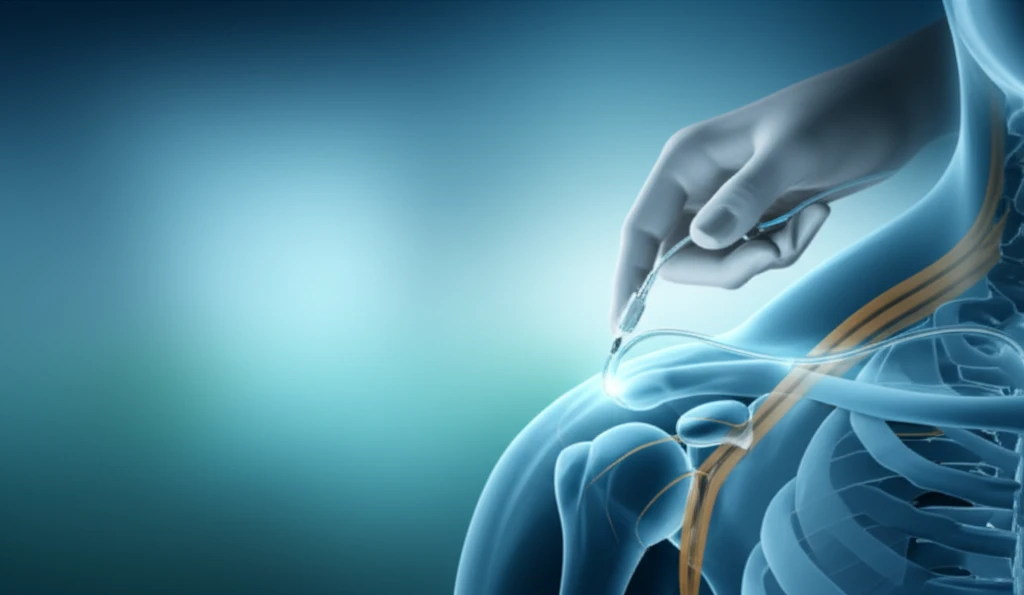
Traditionally, interscalene regional anesthesia, which involves placing a catheter near the nerves in the neck to deliver pain medication, has been a common approach for managing post-operative pain following TSA. However, this method isn't without potential risks. One significant challenge is differentiating between nerve-related complications caused by the surgery itself and those arising from the regional anesthesia.
To address this issue, researchers developed a 'dry catheter' technique. With this approach, the catheter is placed but not immediately activated. A neurovascular examination is performed on the patient immediately after surgery, before any anesthetic is delivered through the catheter. If the exam is normal, the regional anesthesia is then initiated. This allows doctors to determine if any nerve issues were caused by the surgery, prior to starting the nerve block.
How Does the 'Dry Catheter' Technique Work?
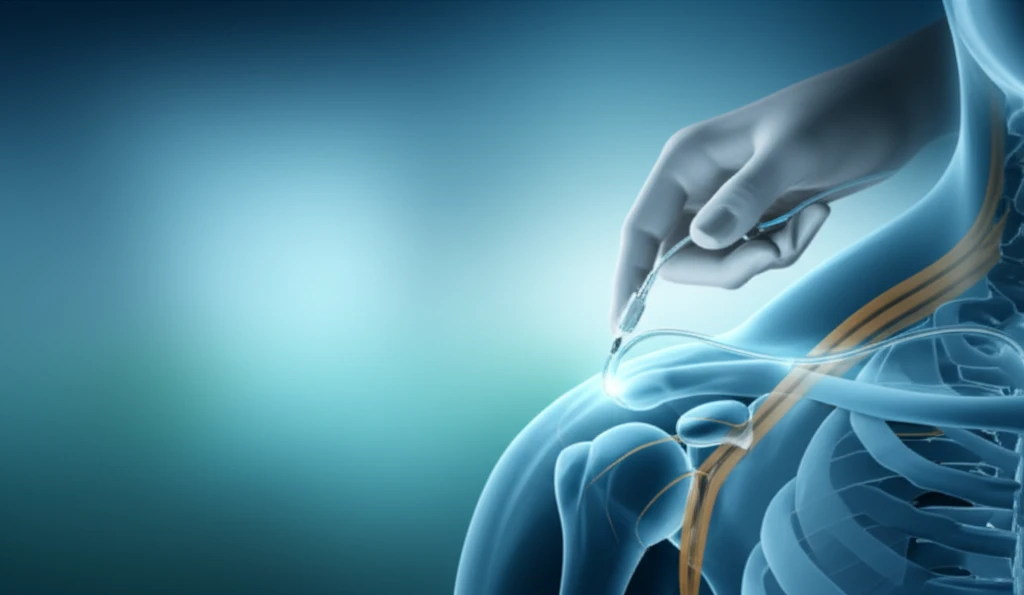
The dry catheter technique represents a strategic shift in how regional anesthesia is administered for shoulder arthroplasty. In a study involving 125 shoulders, doctors placed an interscalene catheter as usual, but they didn't immediately start the medication infusion. Patients underwent their shoulder surgery under general anesthesia, and upon awakening in the recovery room, a comprehensive neurovascular examination was performed. This examination checked for any signs of nerve damage, such as weakness, numbness, or impaired motor function.
- Pre-operative Assessment: Baseline neurological function is evaluated.
- Catheter Placement: An interscalene catheter is placed without immediate activation.
- Post-operative Examination: A thorough neurovascular exam is conducted post-surgery, pre-anesthesia.
- Anesthesia Activation: If the exam is normal, regional anesthesia is initiated; otherwise, alternative pain management is used.
- Monitoring: Pain levels and neurological status are closely monitored throughout recovery.
The Future of Pain Management in Shoulder Arthroplasty
The dry catheter technique represents a valuable step forward in optimizing patient safety and pain control following shoulder arthroplasty. By allowing for a clear distinction between surgical and anesthesia-related nerve issues, this method empowers medical teams to make informed decisions and tailor pain management strategies to individual patient needs. While the study authors ultimately stopped using interscalene anesthesia due to their perceived complication rate, the dry catheter approach offers a framework for other medical centers to refine their protocols and improve patient outcomes in shoulder arthroplasty.
