Securing Rectal Cancer Surgery: How a Nerve Landmark Can Prevent Urethral Injury
"A novel surgical technique uses the autonomic nerve to identify the prostate gland during transanal total mesorectal excision, minimizing the risk of urethral damage."
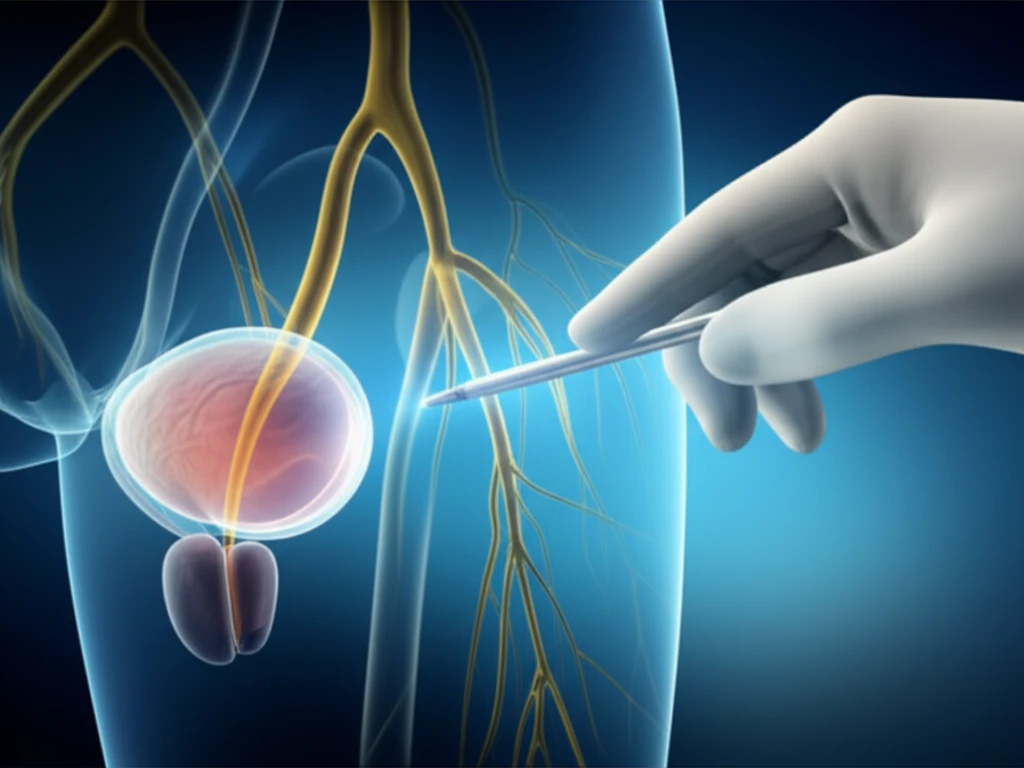
In rectal cancer surgery, protecting the autonomic nerve while achieving complete tumor removal is paramount. This ensures both oncological control and preservation of crucial bodily functions. Laparoscopic surgery, while beneficial, can pose challenges, especially in male patients with obesity or a narrow pelvis, due to limited visibility within the deep pelvic region. This can increase the risk of incomplete mesorectal excision and less favorable oncological outcomes.
Transanal total mesorectal excision (taTME) has emerged as a promising technique to overcome these limitations, offering improved access and visualization. However, it also carries an inherent risk of iatrogenic urethral injury in men, with reported frequencies ranging from 0% to 6.7% in single-center studies and 0.7% in the Low Rectal Cancer Development program.
Urethral injury typically occurs during anterior dissection near the preprostatic urethra, often because surgeons lack sufficient awareness of the intricate anatomy involving the neurovascular bundle of Walsh, the prostate gland, and the rectourethral muscle. Addressing this critical challenge is essential for improving patient outcomes in rectal cancer surgery.
Autonomic Nerve as a Guide: A Step-by-Step Surgical Technique
To address the risk of urethral injury, a novel surgical technique has been developed that uses the autonomic nerve as a landmark to identify the prostate gland and ensure safe dissection of the male rectourethral muscle. This approach aims to enhance precision and minimize the potential for damage during taTME.
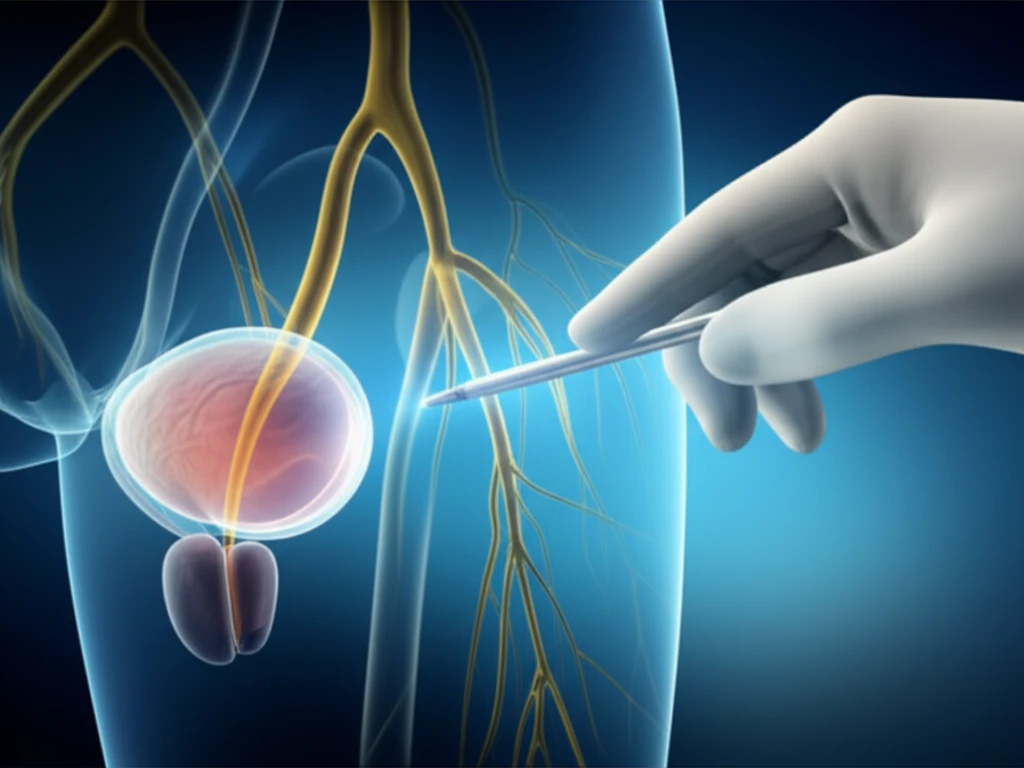
- Initial Dissection: Circumferential rectal dissection begins at the anorectal ring, proceeding posteriorly and cranially within the avascular presacral plane.
- Nerve Identification: Dissection from the posterior wall towards the left side facilitates recognition of the rise of the fourth pelvic splanchnic nerve (S4). This nerve serves as a critical landmark.
- Prostate Identification: By tracing the autonomic nerves anteriorly while carefully identifying S4 and the neurovascular bundle, the prostate gland can be accurately located before dissecting the rectourethral muscle.
- Safe Muscle Dissection: Using this nerve-guided approach, the rectourethral muscle can be safely cut while clearly visualizing the prostate gland, thus avoiding urethral injury. This also allows for precise selection of the cutoff line of the rectourethral muscle based on individual patient anatomy.
Reducing Risks, Improving Outcomes
By adopting this surgical technique, surgeons can significantly reduce the risk of urethral injury during taTME, a critical step towards improving patient safety and outcomes in rectal cancer surgery.
The key lies in using the autonomic nerve as a reliable landmark to guide dissection and accurately identify the prostate gland. This approach enhances precision and control, minimizing the potential for iatrogenic damage.
Further research and widespread adoption of this technique could lead to a new standard of care in rectal cancer surgery, ensuring both effective tumor removal and preservation of vital anatomical structures.
