Second Chance Hearts: Are Younger Donor Hearts the Key to Adult Transplants?
"New research explores if hearts from early adolescent donors can safely expand the donor pool for adult heart transplant recipients, offering hope and better outcomes."
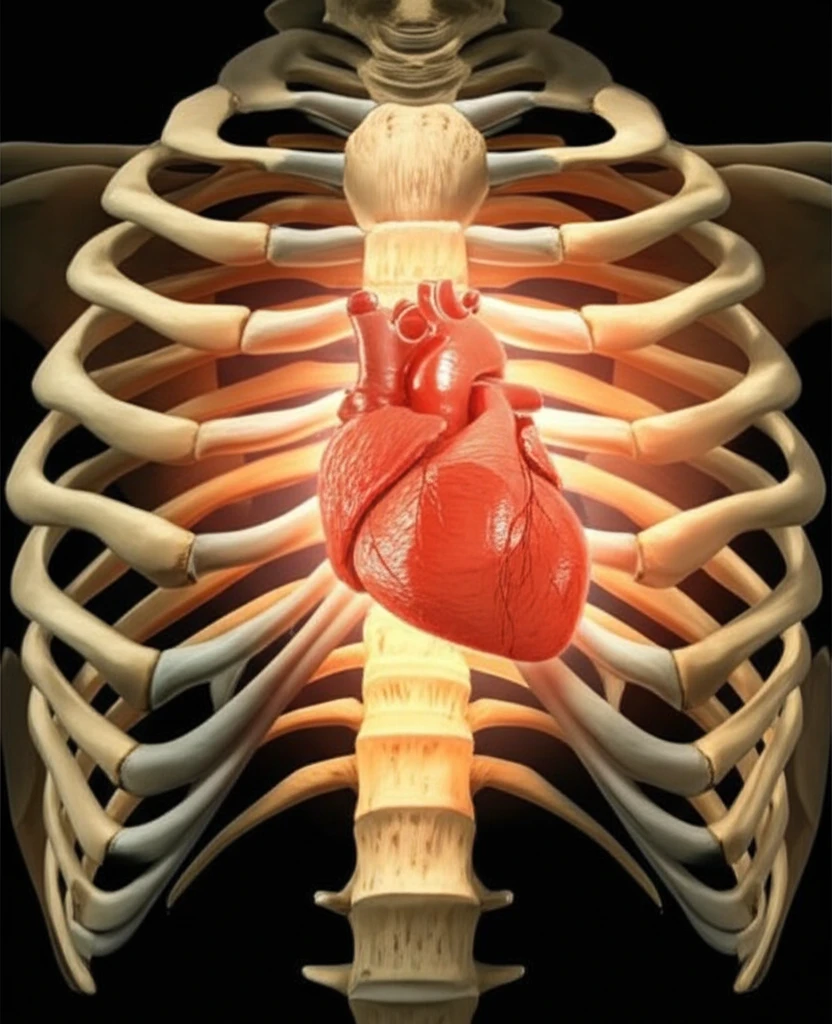
For individuals facing end-stage heart failure, a heart transplant represents more than just a medical procedure; it's a lifeline. While advancements in left ventricular assist devices have provided crucial support, heart transplantation remains the gold standard for extending and improving the quality of life. Unfortunately, the demand for donor hearts far exceeds the supply. It's estimated that over 20,000 people in the United States could benefit from a heart transplant, yet only a fraction receive one each year.
This disparity highlights a critical need to expand the donor pool safely and effectively. One potential solution lies in re-evaluating the use of hearts from early adolescent donors (individuals aged 10 to 14). These hearts, often not considered for pediatric recipients, could offer a valuable resource for adult patients in need. However, concerns about hormonal factors and heart development have historically limited their use.
Now, a groundbreaking study challenges these long-held beliefs. Researchers have delved into the outcomes of adult transplant recipients who received hearts from early adolescent donors, comparing them to those who received hearts from traditional adult donors. The findings may transform how we approach heart transplantation, offering new hope to those on the waiting list.
Breaking Barriers: Examining Early Adolescent Hearts for Adult Transplants
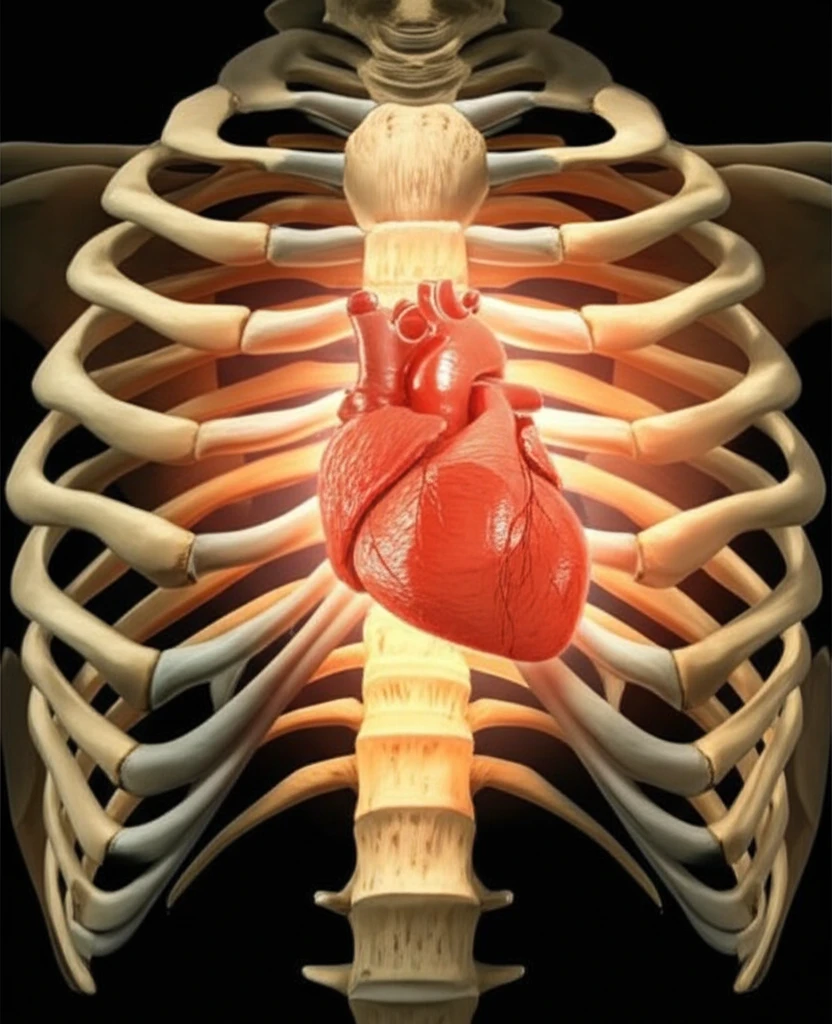
Traditionally, the hearts of early adolescent donors haven't been widely used for adult transplants due to concerns about their development and hormonal activity. Early adolescence is a period marked by significant hormonal changes that fuel growth spurts, sexual development, and the emergence of secondary sexual characteristics. Some experts have theorized that the hormonal surge during this time also impacts heart growth, increasing both the thickness of the heart walls and overall contractility.
- All-cause mortality
- Cardiac allograft vasculopathy (CAV), a condition affecting the blood vessels of the transplanted heart
- Primary graft failure (PGF), which is when the donor heart fails within 90 days of transplant
A Future with More Available Hearts?
This research delivers a powerful message: hearts from early adolescent donors, when carefully matched to adult recipients, can lead to successful outcomes. By expanding the criteria for donor heart acceptance, the medical community can tap into a valuable resource and offer a life-saving treatment to more individuals in need. As transplant centers embrace these findings, the future of heart transplantation looks brighter, with the potential to significantly reduce waiting times and improve the lives of countless patients.
