Scarf Technique Saves the Day: A New Method for Pancreatic Surgery After Gastrectomy
"Learn about the 'jejunal scarf-covering method,' a groundbreaking surgical innovation that prevents pancreatic fistulas in patients undergoing complex abdominal procedures."
Pancreaticoduodenectomy (PD) is a common surgical procedure to treat malignancies of the ampulla of Vater, duodenum, head of the pancreas, and distal common bile duct. The creation of a safe and secure anastomosis (connection) between the pancreas and the small intestine is critical to prevent complications.
One of the most serious complications following PD is the development of a pancreatic fistula (PF). A pancreatic fistula is a leak from the surgical connection, leading to intra-abdominal abscesses, sepsis, hemorrhage, and high mortality. Therefore, surgeons have explored various techniques to reinforce the pancreaticoenterostomy and prevent leakage.
Traditional methods of reinforcing the anastomosis involve wrapping skeletonized vessels and the anastomotic site with materials like the round ligament or greater omentum. However, these options are often unavailable in patients who have previously undergone total gastrectomy, a procedure where these tissues are often removed. This is where the 'jejunal scarf-covering method' comes in, offering a novel solution for these complex cases.
The Jejunal Scarf-Covering Method: A Step-by-Step Guide
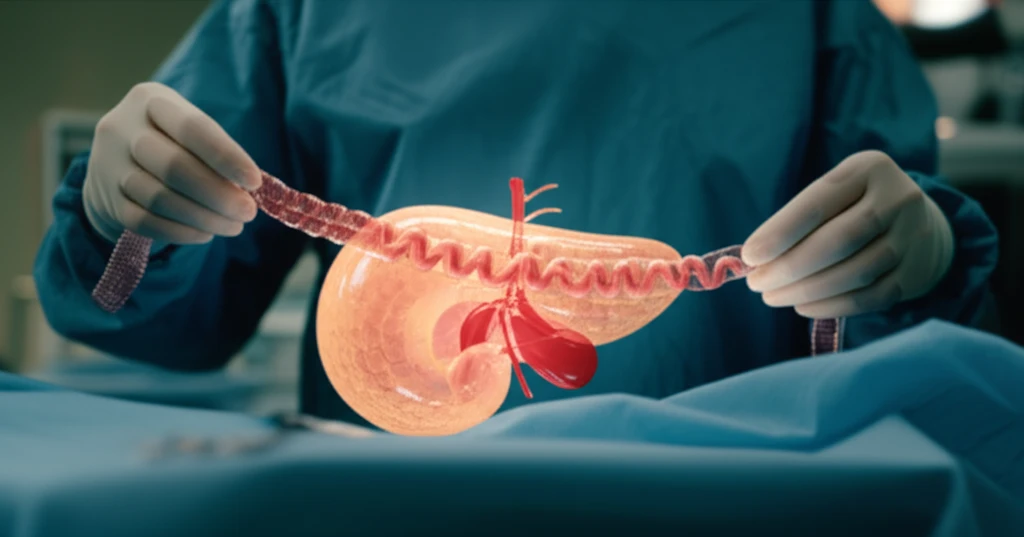
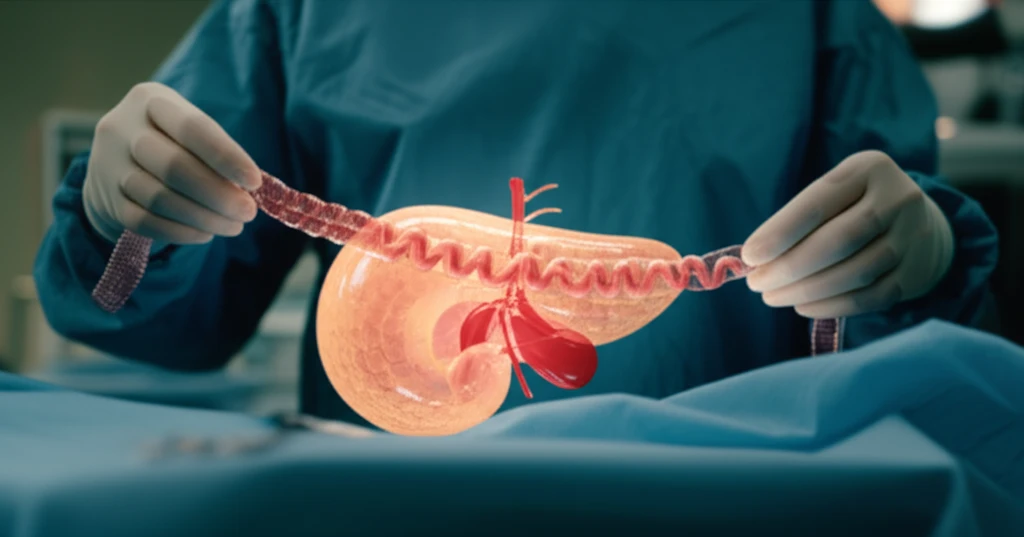
The jejunal scarf-covering method involves using a segment of the jejunum (small intestine) to wrap and reinforce the pancreaticojejunostomy (PJ) site, where the pancreas is connected to the jejunum. This technique is particularly beneficial for patients who have undergone total gastrectomy, as it utilizes the available jejunum to provide additional support and protection to the anastomosis.
- Jejunal Loop Creation: A segment of the proximal jejunum (the portion closest to the stomach) is brought up to the surgical site in a retrocolic position (behind the colon).
- Double Loop Formation: The jejunum is positioned to create a loop, and the sides of the loop are sutured together to form a double-layered structure.
- Pancreaticojejunostomy (PJ): The remnant pancreas, with a stent (tube) inserted into the pancreatic duct, is placed onto this prepared jejunal double loop. A precise, layered anastomosis is then performed to connect the pancreatic duct to the jejunum.
- Jejunal Scarf Wrapping: After the PJ is complete, the portion of the jejunal loop opposite the anastomosis is carefully bent over and wrapped around the PJ site, creating a protective 'scarf.'
- Securing the Wrap: The edges of the jejunal wrap are then sutured to the pancreatic parenchyma (the functional tissue of the pancreas) to ensure it stays securely in place.
- Additional Anastomoses: Finally, the hepaticojejunostomy (connection between the bile duct and jejunum) is performed, and drainage tubes are strategically placed to manage any potential leakage.
The Future of Pancreatic Surgery: Hope for Complex Cases
The jejunal scarf-covering method represents a significant advancement in surgical technique, offering a valuable option for preventing pancreatic fistulas in challenging cases. While further research and long-term studies are needed, this innovative approach holds great promise for improving patient outcomes and reducing the morbidity associated with pancreatic surgery after total gastrectomy.
