SBRT: Revolutionizing Cancer Treatment?
"Unpacking the Latest Advances in Stereotactic Body Radiation Therapy for Lung and Prostate Cancer"
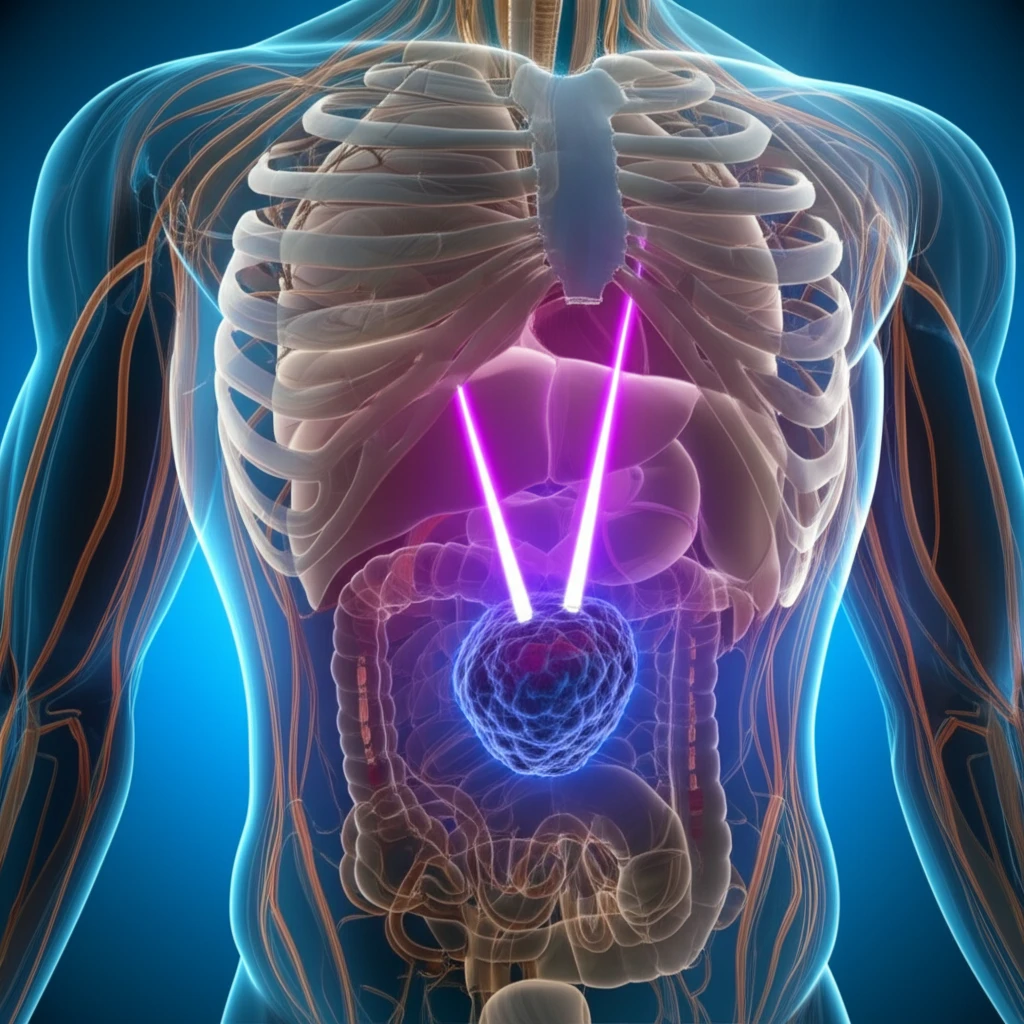
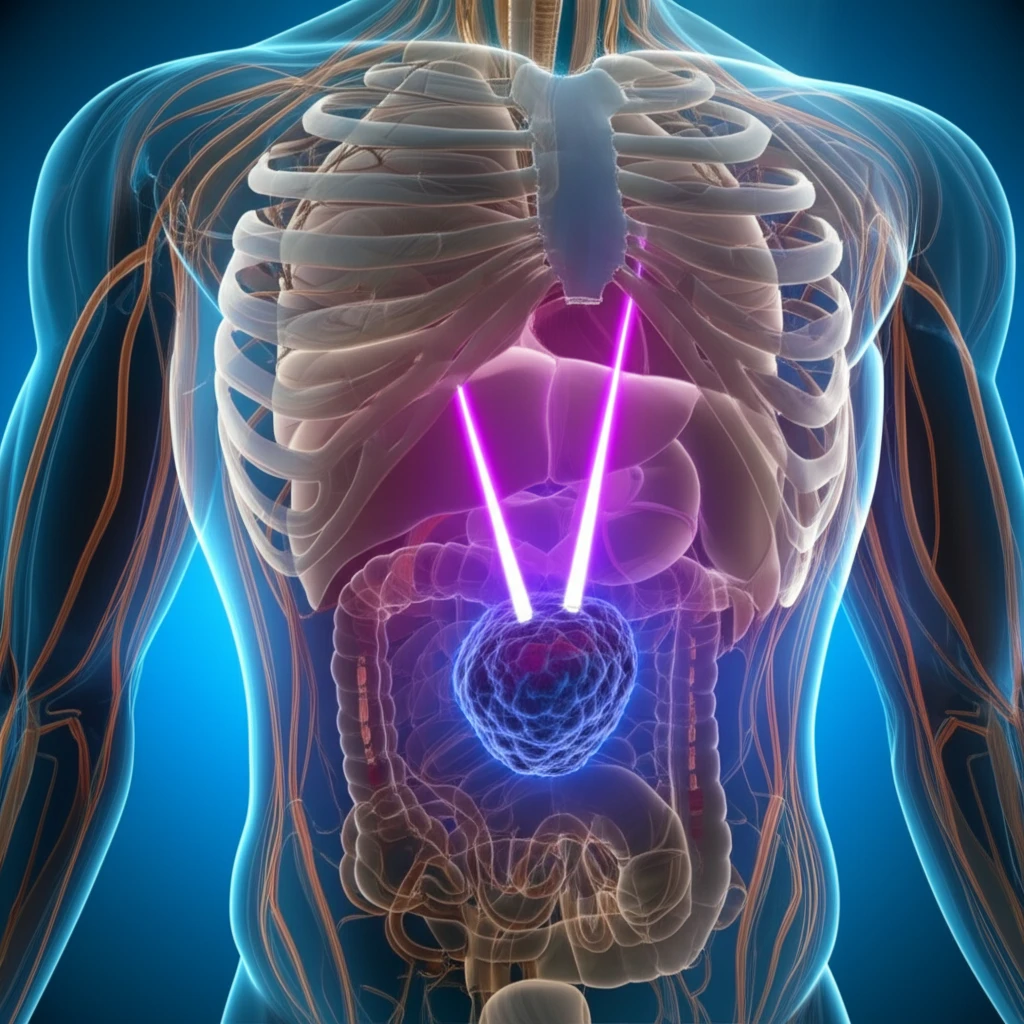
Stereotactic Body Radiation Therapy (SBRT) has emerged as a significant advancement in cancer treatment, offering a precise and effective approach to targeting tumors while minimizing damage to surrounding healthy tissues. This technique is particularly valuable for patients with localized tumors who may not be suitable candidates for surgery or prefer a non-invasive treatment option.
Two key areas where SBRT has shown considerable promise are in the treatment of lung and prostate cancer. In lung cancer, SBRT is used for both primary early-stage non-small cell lung cancer (NSCLC) and local relapses following surgery. For prostate cancer, SBRT offers an alternative to traditional radiation therapy, with the goal of delivering high doses of radiation to the tumor while sparing the rectum and other nearby organs.
This article will explore the latest research on SBRT for lung and prostate cancer, highlighting the benefits, challenges, and ongoing efforts to optimize treatment protocols. We will delve into the importance of credentialing in lung SBRT, as well as the dosimetric considerations for achieving optimal rectal sparing in prostate cancer SBRT. Understanding these aspects is crucial for healthcare professionals and patients alike, as SBRT continues to evolve and play an increasingly important role in cancer management.
Lung SBRT: Credentialing and Consistency in Treatment Delivery
A study was conducted in Canada to assess the variability in lung SBRT practice among different centers. The OCOG-LUSTRE trial (NCT01968941) compared SBRT to conventionally hypofractionated radiation for stage I medically inoperable NSCLC. A key component of this trial was a comprehensive credentialing process aimed at ensuring consistent and high-quality treatment delivery across all participating centers.
- Completing an institutional survey detailing treatment protocols, dosimetry practices, and image guidance equipment.
- Demonstrating acceptable delivery accuracy using the Imaging and Radiation Oncology Core (IROC) thoracic phantom.
- Successfully contouring and completing standardized test cases for both central and peripheral NSCLC tumors.
The Future of SBRT: Balancing Precision and Individualized Care
SBRT is rapidly becoming a cornerstone of modern cancer treatment, offering a non-invasive and highly targeted approach to tumor control. As technology advances and our understanding of cancer biology deepens, SBRT is likely to become even more precise and effective.
Ongoing research is focused on optimizing treatment protocols, minimizing side effects, and personalizing SBRT based on individual patient characteristics. By addressing the challenges of credentialing and dosimetric optimization, we can ensure that all patients have access to the highest quality SBRT treatment, regardless of where they receive care.
The insights into the rectal V3600cGy, highlights the complexity in prostate SBRT planning. As this treatment modality continues to be developed, open research for dose prescriptions and best practice will be necessary.
