ROS1 holds the key to cancer treatment?
"A breakthrough study illuminates how the subcellular location of ROS1 fusion proteins can dictate oncogenic signaling, opening new avenues for targeted therapies."
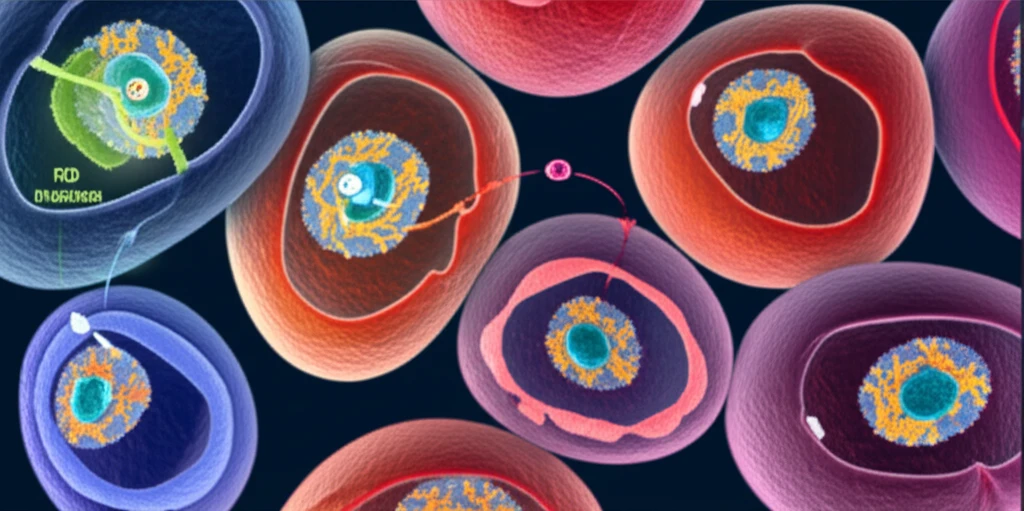
Cancer is often driven by the aberrant hyper-activation of receptor tyrosine kinases (RTKs), which are crucial for cell growth and differentiation. This activation results from various genetic alterations, including gene rearrangements that lead to the formation of fusion proteins. Among these, fusions involving the anaplastic lymphoma kinase (ALK) and ROS proto-oncogene 1 (ROS1) have gained significant attention.
In these fusions, the kinase domain of the RTK is joined in cis to various N-terminal partners. Kinase inhibitors (TKIs) like crizotinib have proven effective in treating cancers driven by these fusions; however, resistance remains a significant challenge, highlighting the need for a deeper understanding of their oncogenic mechanisms.
A crucial aspect of these oncoprotein kinase fusions is how their subcellular localization influences their oncogenic properties. Many oncoprotein fusion kinases, such as ALK and ROS1 variants, acquire subcellular localization signals from their N-terminal partners. This raises the question of whether abnormal subcellular localization significantly contributes to their ability to promote cancer.
How Does Subcellular Localization Regulate Oncogenic Signaling?
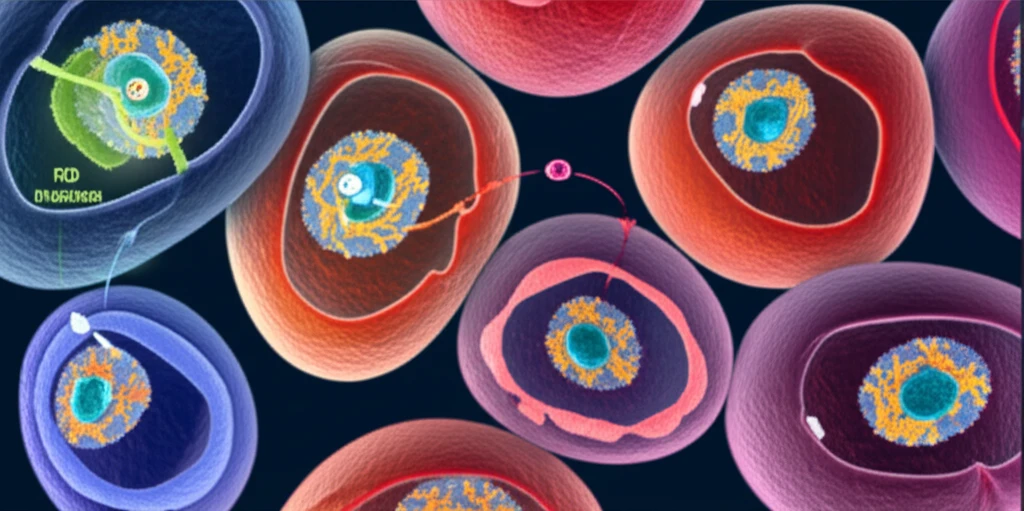
Researchers investigated the differential functional properties of various ROS1 oncoprotein fusions. They engineered a genetically controlled system to express common ROS1 fusion oncoproteins found in patient tumors, including CD74-ROS1, SDC4-ROS1, and SLC34A2-ROS1. A topological analysis indicated that these fusions result in a membrane-anchored, cytoplasmic-facing kinase domain. All three ROS1 fusions showed constitutive kinase activation, as measured by ROS1 phosphorylation.
- SDC4-ROS1 and SLC34A2-ROS1: Fusion oncoproteins localized to endosomes, activating the MAPK pathway.
- CD74-ROS1: Variants localized to the endoplasmic reticulum (ER), showing compromised activation of MAPK.
- FYVE-CD74-ROS1: Re-localization of CD74-ROS1 from the ER to endosomes restored MAPK signaling.
What Does This Mean for Future Cancer Treatments?
These findings demonstrate that the specific N-terminal fusion partners in gene rearrangements involving RTKs can directly control MAPK signaling by influencing subcellular localization. Understanding the subcellular localization of aberrant gene fusion oncoproteins could provide additional avenues for cancer treatment. Targeting these specific localizations may offer more effective and personalized therapeutic strategies, especially in overcoming resistance to existing treatments like crizotinib. Further research into how subcellular localization regulates fusion oncoprotein activity could lead to new biomarkers and therapeutic targets, improving outcomes for cancer patients.
