RFA: A Ray of Hope for Liver Metastasis from Gastric Cancer?
"Discover how radiofrequency ablation (RFA) is changing the game for patients with metastatic liver tumors originating from gastric cancer. Is it the breakthrough we've been waiting for?"
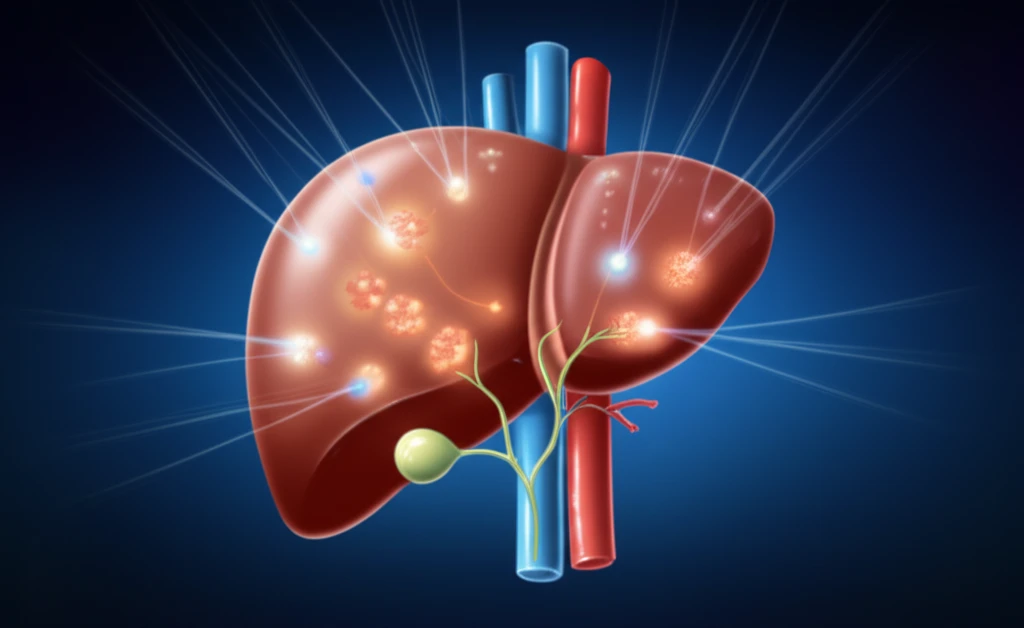
Gastric cancer remains a significant global health challenge, particularly in Asia, where it's a leading cause of cancer-related deaths. One of the most daunting complications is the spread of cancer to the liver, known as liver metastasis. This condition has historically presented limited treatment options and poor prognoses.
Traditional treatments, such as chemotherapy, have been the standard of care for metastatic liver tumors. However, these systemic treatments often come with significant side effects and may not always be effective in eradicating the tumors completely. As a result, there's been a growing need for more targeted and less invasive approaches.
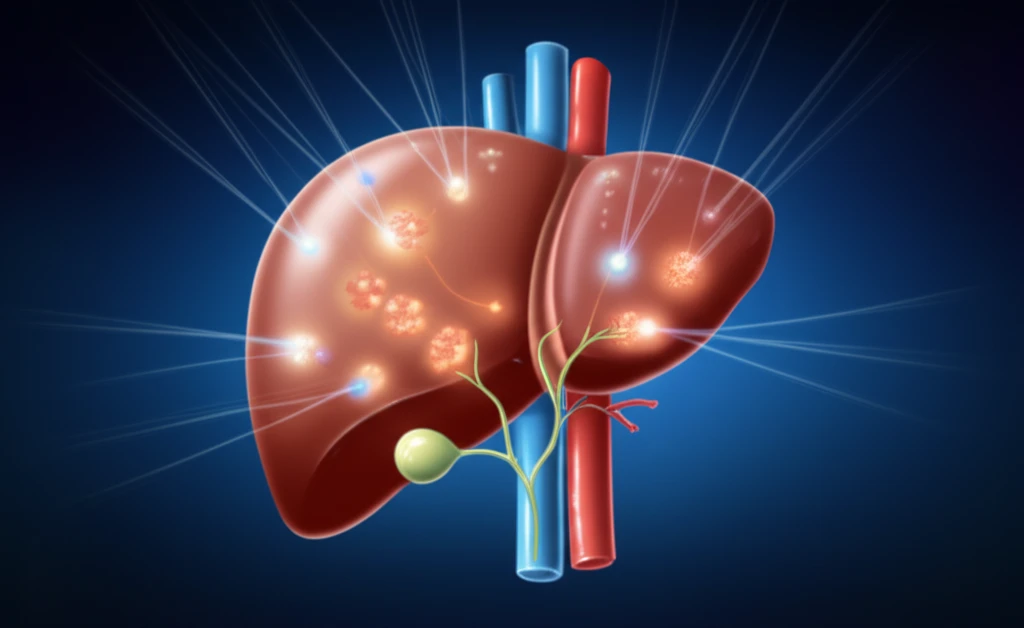
Enter radiofrequency ablation (RFA), a minimally invasive technique that uses heat to destroy cancer cells. RFA has emerged as a promising alternative for treating liver tumors, but its effectiveness specifically for metastases originating from gastric cancer has been less explored. Recent research is shedding light on the potential of RFA to transform the treatment landscape for these patients.
The RFA Revolution: How It Works and Why It Matters
Radiofrequency ablation (RFA) is a sophisticated procedure that utilizes high-frequency electrical currents to generate heat and destroy cancer cells. During RFA, a specialized needle electrode is inserted directly into the tumor, guided by imaging techniques such as ultrasound or CT scan. Once in place, the electrode emits radiofrequency energy, creating a zone of intense heat that effectively 'cooks' the tumor cells.
- Precision Targeting: RFA allows doctors to target tumors with pinpoint accuracy, minimizing damage to surrounding healthy tissue.
- Minimally Invasive: The procedure requires only a small incision, leading to less pain and quicker recovery.
- Reduced Side Effects: Compared to chemotherapy, RFA typically has fewer systemic side effects.
- Outpatient Procedure: In many cases, RFA can be performed on an outpatient basis, allowing patients to return home the same day.
The Future of Liver Metastasis Treatment: A Glimmer of Hope
The findings of the study highlight the significant potential of RFA as a valuable tool in the fight against metastatic liver tumors from gastric cancer. While further research is always needed to refine treatment protocols and identify the best candidates for RFA, the results offer a promising glimpse into the future of cancer therapy. As technology advances and our understanding of cancer deepens, innovative approaches like RFA will continue to play a crucial role in improving patient outcomes and transforming lives.
