Revolutionizing Recovery: The Innovative Surgical Solution for Rectovaginal Fistulas
"A groundbreaking technique offers new hope for women suffering from a rare but debilitating complication of rectal cancer treatment."
Rectovaginal fistulas, abnormal connections between the rectum and vagina, present a significant challenge for women, often resulting from complications following rectal cancer surgery. These fistulas can lead to distressing symptoms such as fecal incontinence and chronic infections, severely impacting a woman's physical and emotional well-being. Traditional treatments have varied, with outcomes sometimes unpredictable, creating a need for more effective and reliable solutions.
The medical community has been actively seeking innovative surgical techniques to address this difficult condition. Recent advancements offer new hope through an approach that merges established surgical principles with modern techniques. This involves a combination of identifying and treating the fistula, coupled with reinforcement of the repair to ensure long-term success.
This article delves into a groundbreaking surgical technique that has shown promising results. It explores the philosophy behind this innovative method, including the meticulous steps of the procedure, the expected outcomes, and its potential to significantly enhance the lives of those affected by rectovaginal fistulas. We aim to provide a comprehensive overview that empowers women to understand their options and make informed decisions about their care.
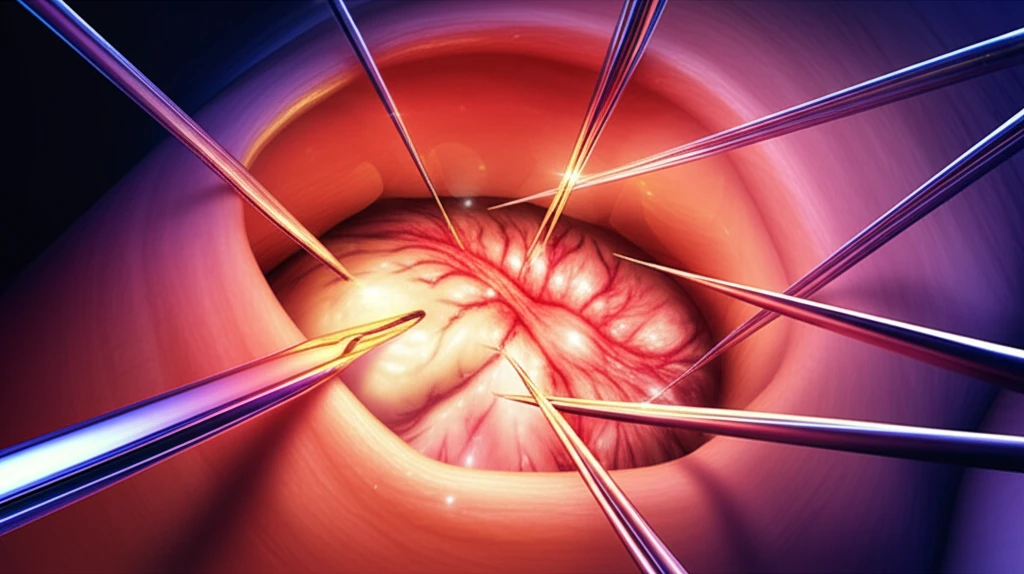
Unveiling the Innovative Surgical Approach: A Step-by-Step Guide
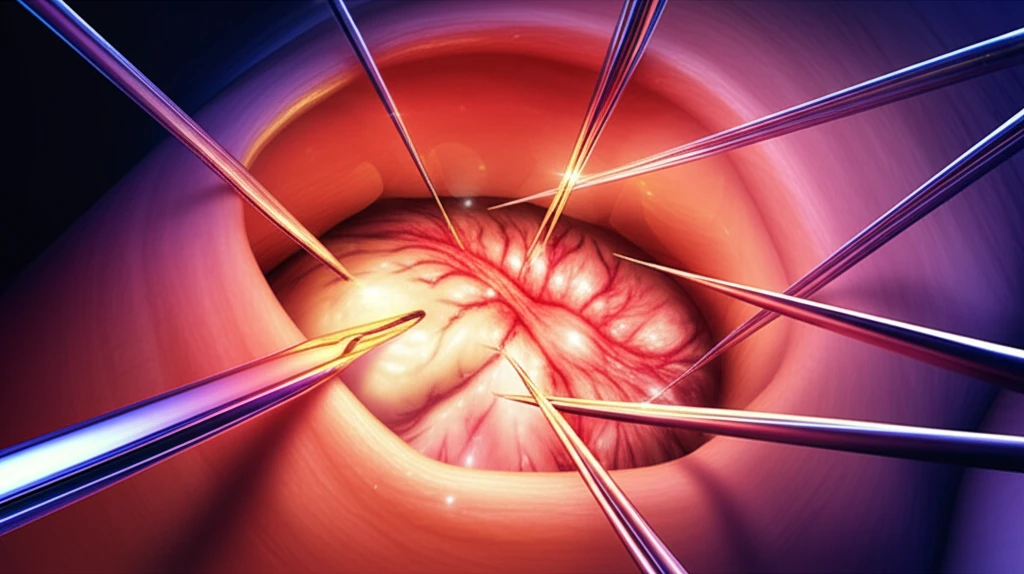
The core of this innovative technique centers on a modified Martius graft combined with a LIFT (Ligation of Intersphincteric Fistula Tract) procedure-inspired strategy. This approach addresses the fistula directly while fortifying the repair site to prevent recurrence. The surgeon begins by carefully identifying the fistulous tract, a critical first step. This involves a thorough examination to map the exact pathway of the fistula, ensuring that all abnormal connections are precisely located.
- Precise identification and mapping of the fistulous tract.
- Ligation and division of the tract to sever the abnormal connection.
- Posterior interposition of a modified Martius graft for reinforcement.
- Meticulous surgical technique to ensure optimal healing.
- Careful post-operative management.
Empowering Women with Knowledge and Hope
This innovative surgical technique represents a significant step forward in the treatment of rectovaginal fistulas. By combining the principles of fistula identification and ligation with the robust reinforcement of a modified Martius graft, this approach offers new hope to women. This technique demonstrates the importance of continuous innovation, patient-centered care, and the ongoing pursuit of better outcomes. It's a powerful example of medical advancements that dramatically improve the lives of those affected.
