Rare Connections: When Aortitis Meets Sweet's Syndrome
"Unveiling a Unique Case Study Linking Two Uncommon Conditions"
In the complex world of medicine, rare associations between different conditions can present unique challenges for diagnosis and treatment. A recent case study sheds light on one such association: the co-occurrence of aortitis and Sweet's syndrome.
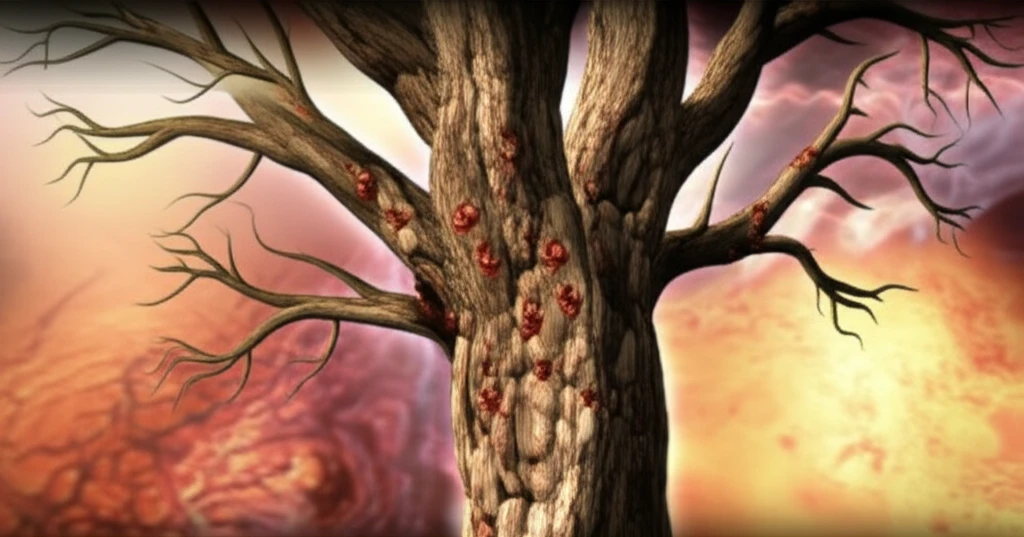
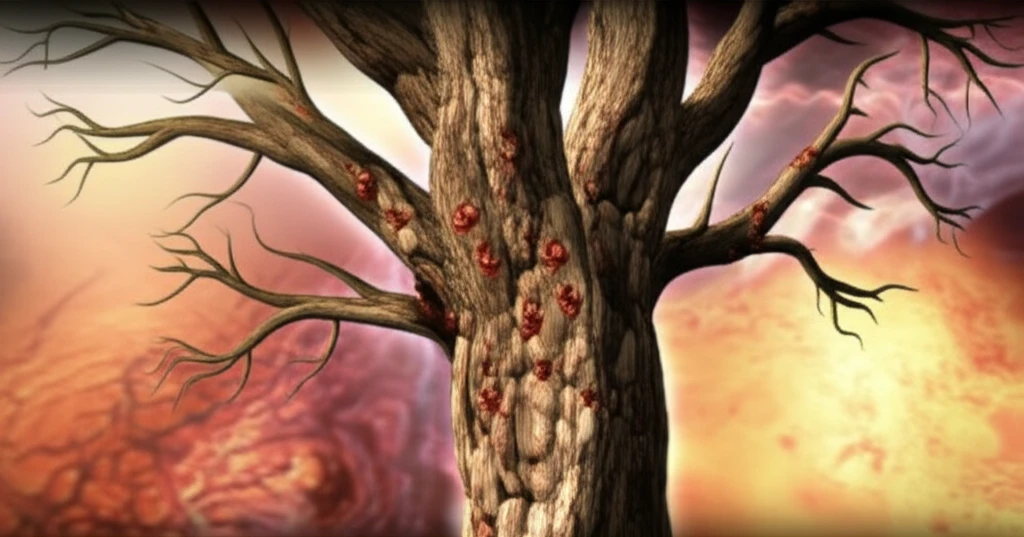
Aortitis, an inflammation of the aorta, the body's largest artery, can lead to serious complications if left untreated. Sweet's syndrome, also known as acute febrile neutrophilic dermatosis, is a rare inflammatory disorder characterized by painful skin lesions and fever. While both conditions are uncommon on their own, their simultaneous occurrence is exceedingly rare.
This article delves into a fascinating case report that explores the diagnosis, treatment, and implications of this unusual medical intersection. By examining the details of this case, we can gain a deeper understanding of the complexities of inflammatory conditions and the importance of considering rare associations in clinical practice.
The Case: A 67-Year-Old Woman's Unexpected Diagnosis
The case study focuses on a 67-year-old woman with no significant past medical history who presented with sudden abdominal pain. Initially assessed in visceral surgery, an abdominal CT scan revealed aortitis, which was subsequently confirmed by an MRI. This prompted her transfer to the internal medicine service for further evaluation.
- Diagnostic Investigations: Extensive testing was conducted to determine the cause of the aortitis. Blood cultures, syphilis serology, and tuberculosis screening were all negative. A temporal artery biopsy was also normal. However, a skin biopsy confirmed the diagnosis of Sweet's syndrome.
- Diagnosis and Treatment: Based on the clinical and pathological findings, the patient was diagnosed with inflammatory aortitis, consistent with Horton's disease (giant cell arteritis), associated with Sweet's syndrome. Treatment was initiated with high-dose corticosteroids (1 mg/kg/day) and an antiplatelet agent.
- Positive Outcomes: The patient's condition improved with treatment. Her overall condition, skin lesions, and biological abnormalities all resolved.
Implications and Future Research
This case emphasizes the importance of considering rare associations in clinical practice. While Sweet's syndrome and aortitis are individually uncommon, their co-occurrence can present unique diagnostic and therapeutic challenges. Further research is needed to better understand the underlying mechanisms that link these conditions and to develop optimal treatment strategies. By recognizing these rare associations, clinicians can improve diagnostic accuracy and provide more effective care for patients with complex inflammatory disorders.
