Rare Cause of Dysphagia: A Tracheal Diverticulum Case
"Unveiling the mysteries of dysphagia: A 61-year-old woman's journey with a tracheal diverticulum"
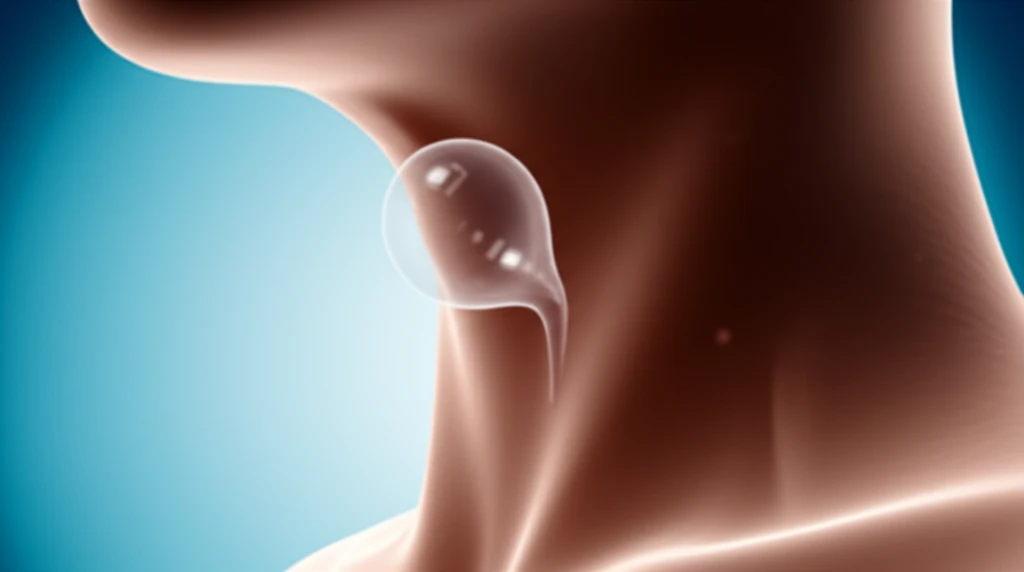
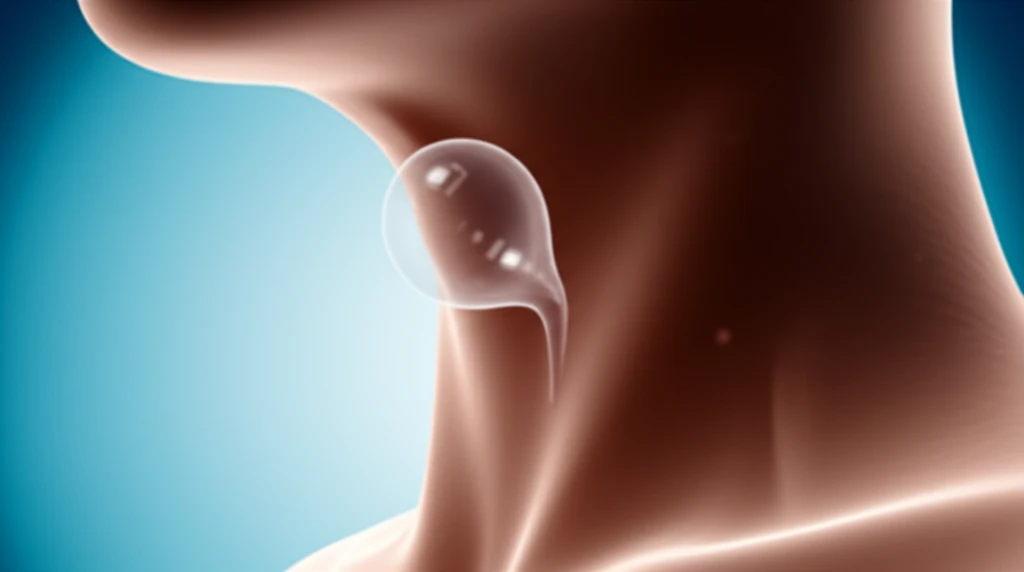
Tracheal diverticula, characterized by small, air-filled invaginations in the paratracheal area, represent a rare clinical entity. These diverticula can manifest as single or multiple occurrences. Although autopsy findings suggest an incidence of approximately 1%, recent investigations utilizing chest computed tomography (CT) have reported prevalence rates ranging from 2% to 3.7% in patients undergoing evaluation.
The presentation of tracheal diverticula is often nonspecific, complicating the diagnostic process. Ideally, computed tomography (CT) imaging studies are used to confirm the diagnosis, followed by surgical resection as the treatment of choice.
In this article, we present a case of a 61-year-old woman with an acquired tracheal diverticulum, with dysphagia as the only presenting symptom. This case underscores the importance of considering rare etiologies in the evaluation of dysphagia and highlights the role of imaging studies and surgical intervention in the management of tracheal diverticula.
Unusual Presentation: A Case of Acquired Tracheal Diverticulum
A 61-year-old female sought medical attention due to gradually worsening dysphagia experienced over a period of three years. Her medical history included hypertension and constipation, managed with antihypertensive medication and psyllium, respectively. Additionally, she had undergone a thyroidectomy 30 years prior. The patient reported iron deficiency anemia and had been prescribed oral iron supplements for three months.
- Surgical Intervention: An incision was made parallel to the anterior border of the sternocleidomastoid. Careful dissection enabled identification of the esophagus and recurrent laryngeal nerve on the right side. The proximal esophagus was identified and encircled with a tape. The tracheal diverticulum, located longitudinally, exerted posterolateral compression on the esophagus. Delineation of the tracheal diverticulum was achieved through positive-pressure insufflation, followed by division of the diverticulum. The posterior tracheal walls were approximated using interrupted 2/0 polydioxanone sutures.
- Pathological Findings: Gross examination of the specimen revealed a single 8 × 0.5-cm light brown tissue sample. Microscopic analysis revealed a fragment of fibrovascular tissue characterized by smooth muscle bundles, dilated and congested blood vessels, adipose tissue, and seromucinous glands, lined by ciliated respiratory mucosa, confirming the diagnosis of tracheal diverticulum. The patient was discharged on the third postoperative day, with subsequent esophagography demonstrating no contrast leak.
Tracheal Diverticula: What We've Learned
In conclusion, tracheal diverticula, though rare, should be considered in the differential diagnosis of dysphagia, particularly when conventional etiologies have been excluded. A high index of clinical suspicion, coupled with appropriate imaging studies, is essential for accurate diagnosis and timely management. Surgical excision remains the treatment of choice for symptomatic diverticula, offering the potential for complete resolution of symptoms and improved quality of life.
