PSC Strictures: Metals, Magnets, or Liver Transplant?
"A Guide to Managing Primary Sclerosing Cholangitis"
Primary sclerosing cholangitis (PSC) is a chronic liver disease where the bile ducts, both inside and outside the liver, become inflamed and scarred. This scarring leads to narrowing (strictures) and widening (dilation) of the bile ducts. Unfortunately, there's no cure for PSC, and liver transplantation is often the last resort for patients with severe complications.
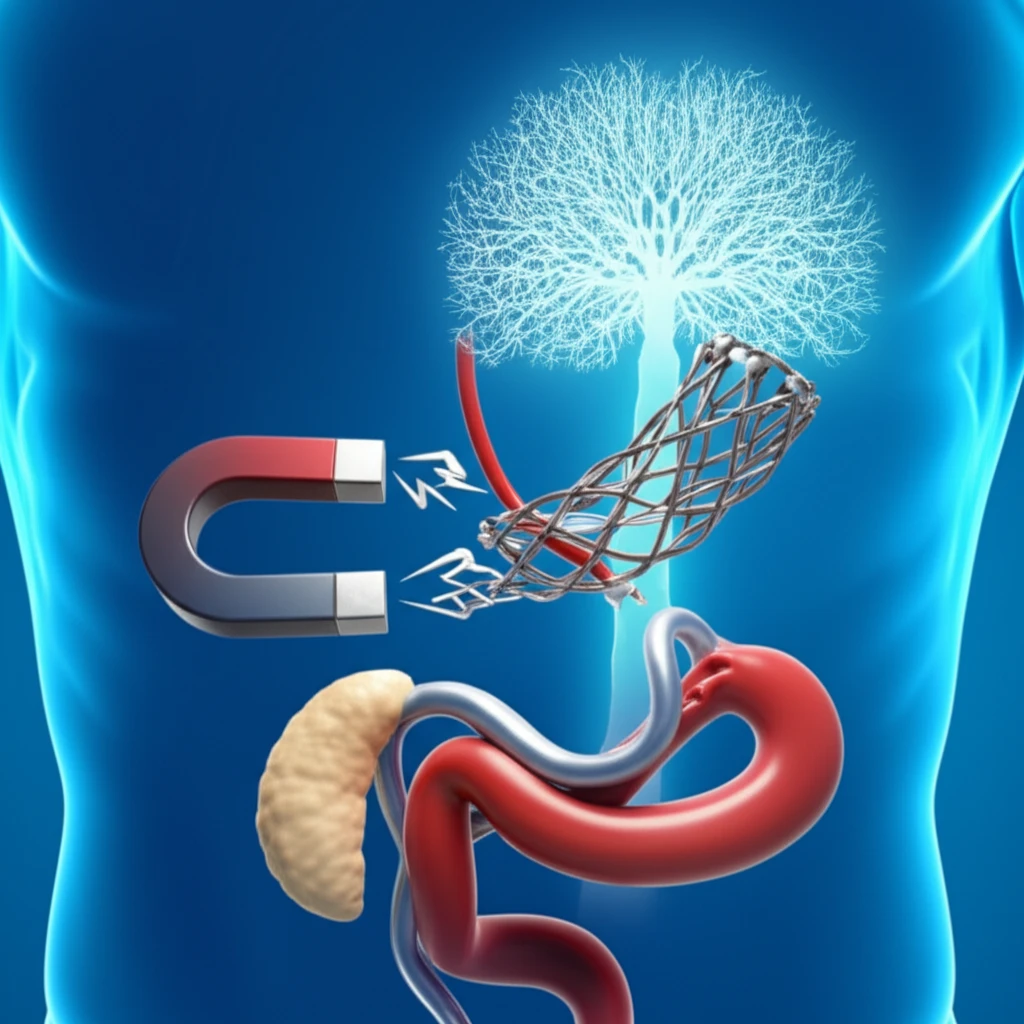
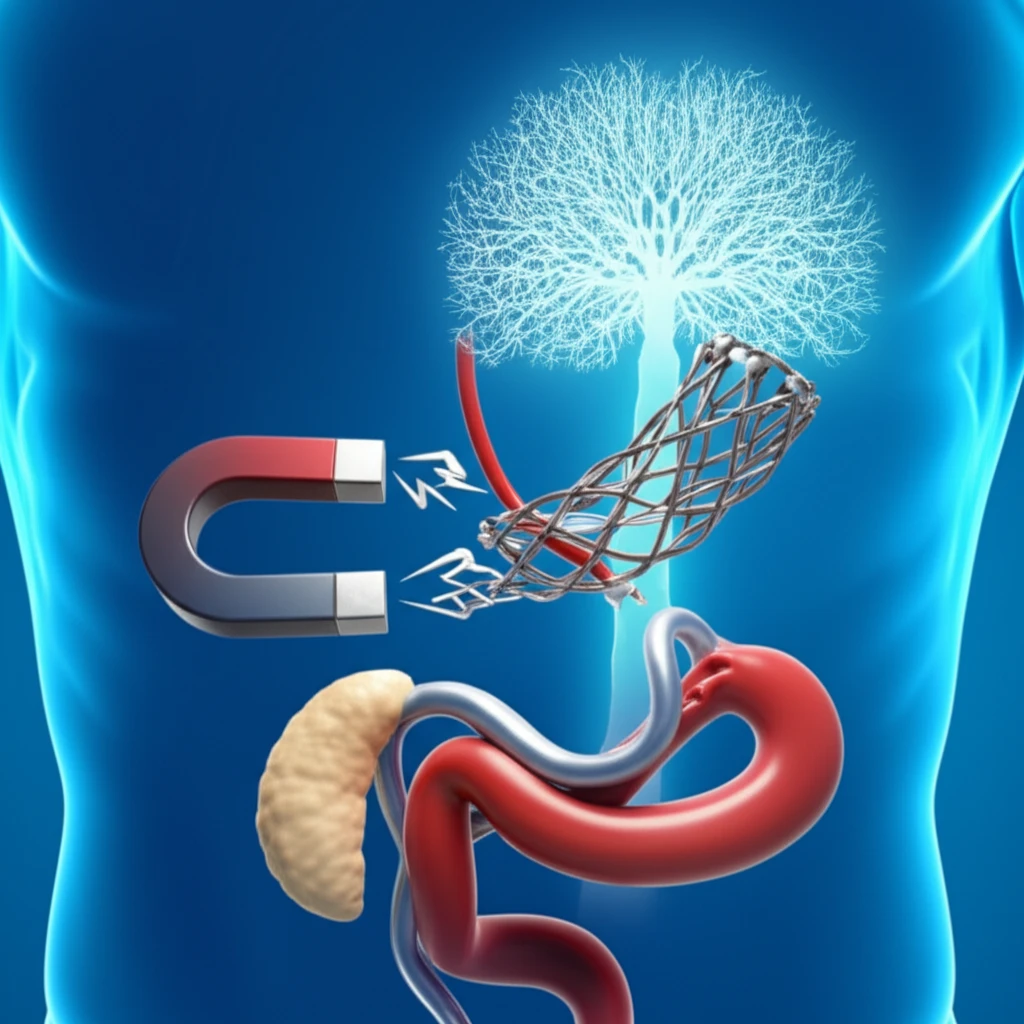
A common problem in PSC is the development of "dominant" strictures, which are significant narrowings that can block bile flow and cause symptoms. Therapeutic endoscopists play a critical role in managing these strictures, using various techniques to improve bile duct patency. These methods include sampling for cancer detection, balloon dilation to widen the strictures, and temporary stent placement to keep the ducts open.
This article explores the latest strategies for managing PSC-related strictures, focusing on endoscopic approaches, including newer techniques like self-expanding metal stents and magnetic compression anastomosis. It also discusses the crucial decision of when to consider liver transplantation.
Endoscopic Strategies for PSC Strictures: Dilation, Stents, and Beyond
Endoscopic retrograde cholangiopancreatography (ERCP) plays a vital role in managing dominant strictures in PSC. While guidelines recommend magnetic resonance cholangiopancreatography (MRCP) as the primary diagnostic tool to avoid ERCP-related complications, ERCP becomes necessary when MRCP is unclear or to treat identified strictures.
- Balloon dilation: Widening the stricture using a balloon catheter.
- Temporary Stenting: Placing plastic stents to maintain patency after dilation. Stents are usually removed after a few weeks to minimize complications like cholangitis.
- Sampling: Obtaining brush cytology or intraductal biopsies to rule out cholangiocarcinoma (CCA).
- Biliary sphincterotomy: May be performed to ensure enough space for stent passage, but it can increase complication risks.
The Future of PSC Management: A Personalized Approach
Managing PSC strictures requires a multifaceted approach. While endoscopic techniques like balloon dilation and temporary stenting remain the cornerstone of treatment, newer modalities like metal stents and magnetic compression anastomosis hold promise but are still investigational.
Liver transplantation remains the ultimate solution for patients with advanced PSC, but optimal timing is crucial. Early diagnosis of cholangiocarcinoma is critical, but even with early detection, the shortage of donor organs can limit the benefits. Biomarkers and genetic studies are helping refine our ability to predict disease progression and identify patients who would benefit most from transplantation.
Ongoing research and collaboration are essential to improve outcomes for individuals with PSC. A multidisciplinary approach, involving hepatologists, endoscopists, and transplant surgeons, is critical for optimal management and improved quality of life.
