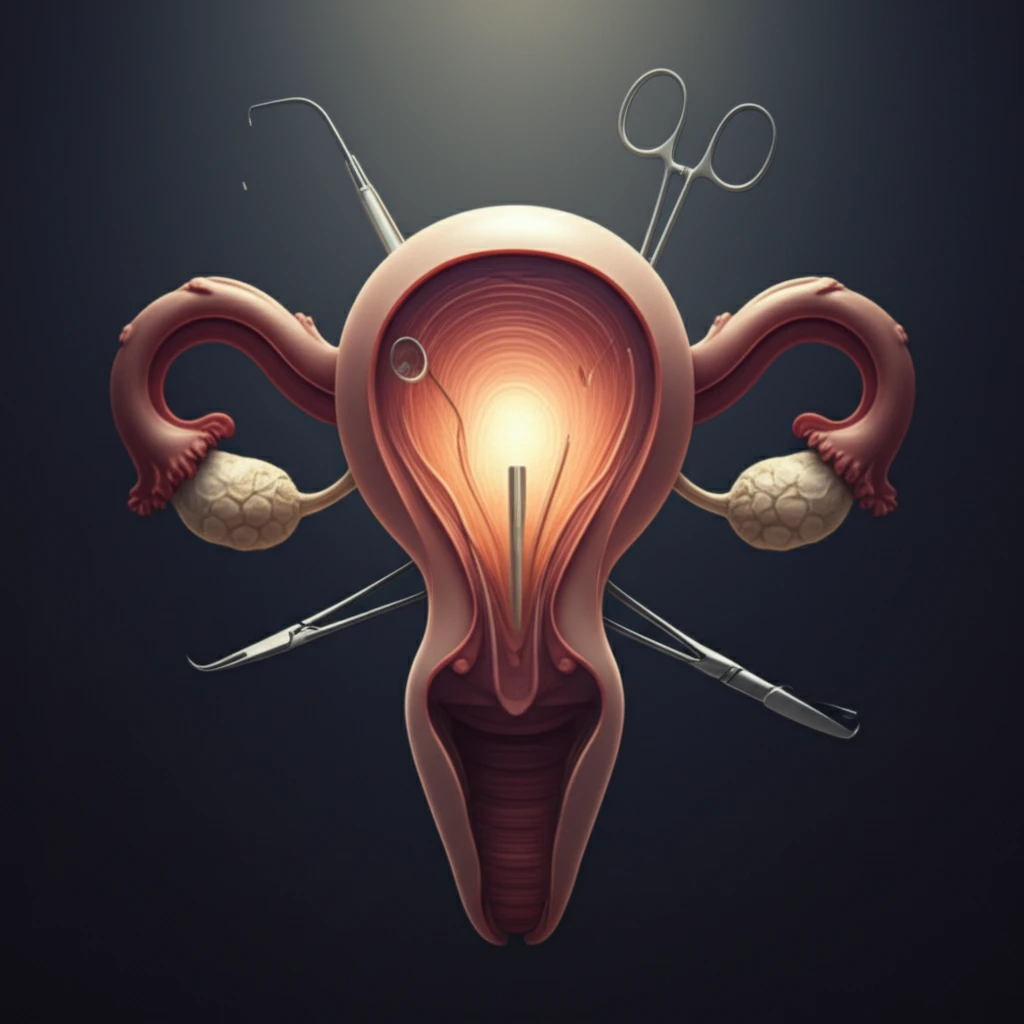
Postpartum Hemorrhage: A Comprehensive Guide to Surgical Management
"When medical interventions aren't enough: Exploring surgical options to manage and treat postpartum hemorrhage."
Postpartum hemorrhage (PPH), or excessive bleeding after childbirth, is a serious complication that can lead to significant maternal morbidity and mortality. While prevention and initial medical management are crucial, surgical intervention becomes necessary when these measures fail to control the bleeding effectively.
This article aims to provide a comprehensive overview of the surgical management of PPH, outlining the essential steps for preparation, resource mobilization, and a systematic approach to evaluation and treatment. We'll explore various fertility-preserving surgical techniques and discuss the critical decision-making process for when a hysterectomy is the only life-saving option.
Understanding the different surgical approaches and knowing when to implement them can significantly improve outcomes for women experiencing PPH. This guide will equip healthcare providers and expectant parents with valuable knowledge to navigate this challenging situation.
Understanding the '4 Ts' of Postpartum Hemorrhage: A Surgical Perspective
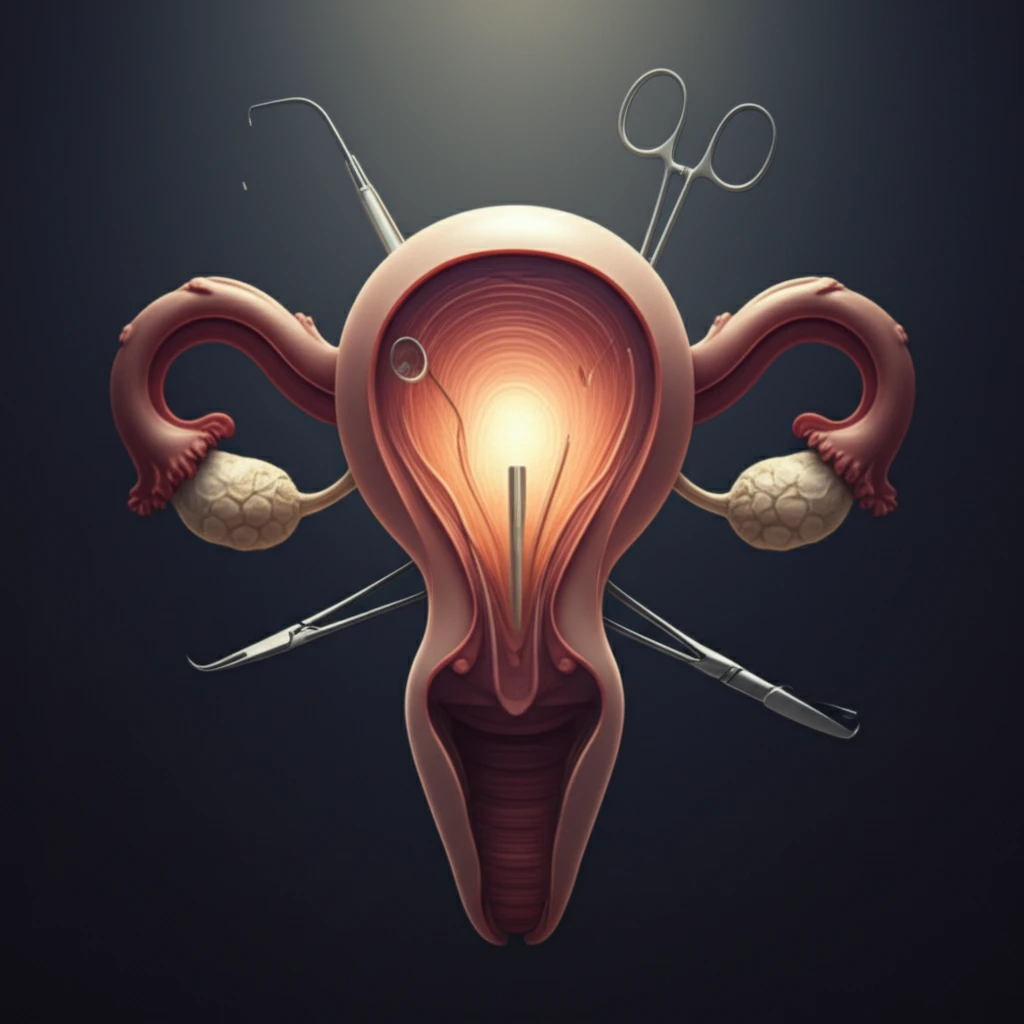
The approach to managing PPH surgically often revolves around addressing the "4 Ts": Tone (uterine atony), Trauma (lacerations), Tissue (retained placental fragments), and Thrombin (coagulation disorders). Surgical interventions are designed to improve uterine tone, remove retained tissue, repair trauma, and control blood loss.
- Restoring uterine contractility by removing tissue and repairing trauma.
- Decreasing blood loss, allowing uterotonic medications to take effect.
- Providing tone through internal or external tamponade.
The Importance of Readiness: When Hysterectomy is the Definitive Solution
While conservative, fertility-sparing surgical approaches are valuable tools in managing PPH, it is crucial to recognize when a hysterectomy becomes necessary. In a hemodynamically unstable patient, team readiness for definitive management with a hysterectomy is essential to reduce the risk of maternal mortality. This decision should be made promptly and decisively, based on the patient's overall condition and response to other interventions.
