PCOS Overdiagnosis: Are We Unnecessarily Labeling Women?
"Explore the expanding diagnostic criteria for Polycystic Ovary Syndrome (PCOS) and the potential risks of overdiagnosis, especially for younger women and those with milder symptoms."
Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder impacting women of reproductive age, associated with infertility, metabolic, cardiovascular, and psychosocial challenges. Women may experience anovulation, irregular menstruation, polycystic ovaries, and signs of androgen excess, which vary based on factors like weight and ethnicity.
Diagnostic criteria for PCOS have broadened over time, leading to an increased number of women being diagnosed. This raises concerns about potential overdiagnosis, which could result in unnecessary disease labeling. This article addresses the potential areas of overdiagnosis and delves into the evidence and uncertainties surrounding the diagnosis and overdiagnosis of PCOS.
Originally described in 1935 through a case series involving seven women with amenorrhea and infertility linked to multiple ovarian cysts, current diagnostic criteria for PCOS include the NIH criteria established in 1990, the Rotterdam criteria that added sonographic presence of polycystic ovaries, and the Androgen Excess and PCOS Society criteria.
The Diagnostic Controversy: Expert Opinion vs. Evidence-Based Definition
Both the NIH and Rotterdam criteria are primarily rooted in expert opinion, facing criticism due to limited high-quality evidence on long-term follow-up or therapeutic benefits. These limitations challenge the ability to create an evidence-based definition of the syndrome. Complicating matters further, studies often fail to differentiate between PCOS phenotypes when reporting associations between PCOS and long-term complications or treatment benefits.
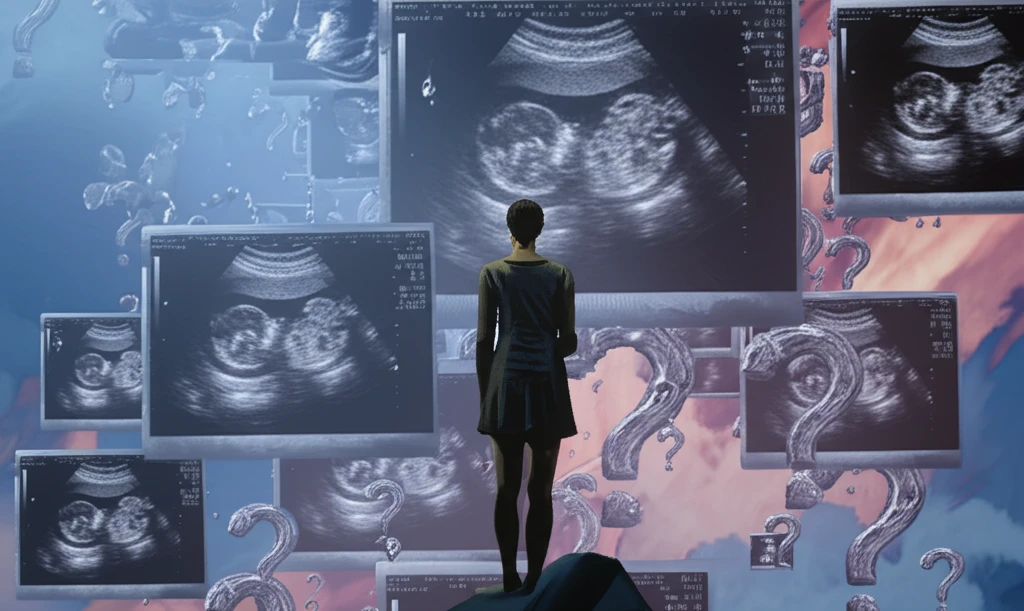
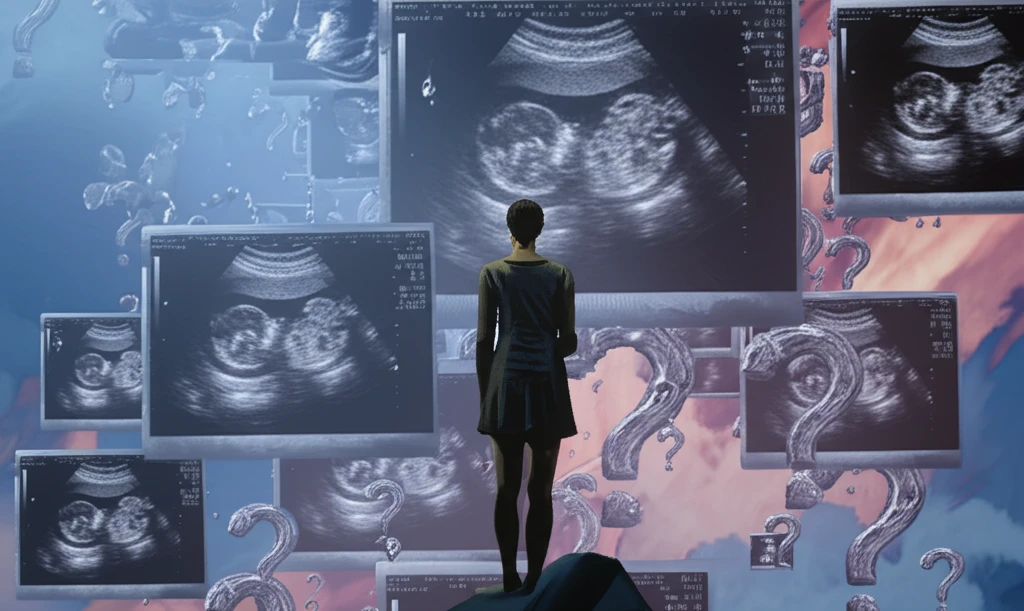
- Including polycystic ovaries as a key diagnostic criterion has faced criticism because they are present in many women without PCOS.
- Features of polycystic ovaries on ultrasonography have been found in 62-84% of women aged 18-30 in the general population and in 7% of women aged 41-45 years.
Moving Forward: Balancing Benefits and Harms
A PCOS label might not be needed to effectively treat many symptoms of PCOS, as the label often does not change the type or intensity of the intervention. A slower, stepped, or delayed approach to diagnosis could optimize benefits and reduce harm from disease labeling, ensuring that each woman's unique circumstances are carefully considered.
