Pancreatic Cancer Treatment: Is Surgical Restaging Always Necessary?
"Experts debate the role of staging laparoscopy in managing locally advanced pancreatic cancer after chemotherapy and radiation."
The optimal management of locally advanced pancreatic cancer (LAPC) remains a topic of considerable debate among oncologists. A key point of contention is whether surgical restaging, specifically staging laparoscopy, is always necessary after patients undergo concurrent chemoradiation therapy. This approach combines chemotherapy and radiation to shrink the tumor before a potential surgical resection.
A recent exchange in the Journal of Korean Medical Science highlights this very issue. Dr. Karabicak raised concerns about the accuracy of determining whether LAPC is truly localized and resectable using current imaging techniques alone. They advocated for staging laparoscopy as a crucial step to rule out any hidden, minute metastases (cancer spread) that might not be visible on standard scans.
In response, Drs. Woo Hyun Paik and Yong-Tae Kim acknowledged the limitations of current imaging but questioned the absolute necessity of staging laparoscopy in all cases. Their argument centers on the high rates of recurrence even after successful resection and the proven benefits of adjuvant chemotherapy, suggesting that micrometastases may be present even in seemingly resectable cancers.
The Role of Staging Laparoscopy: Essential or Optional?
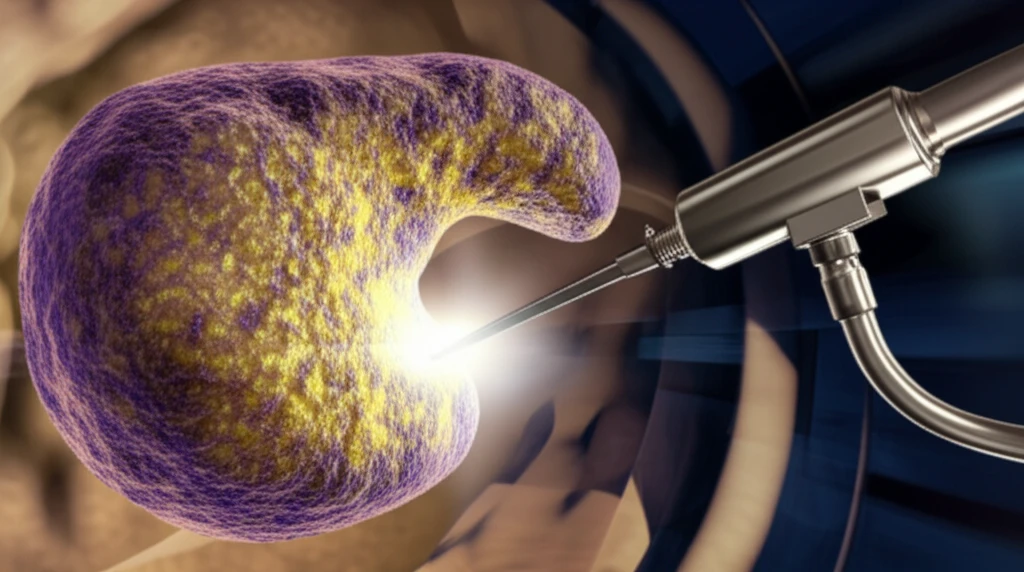
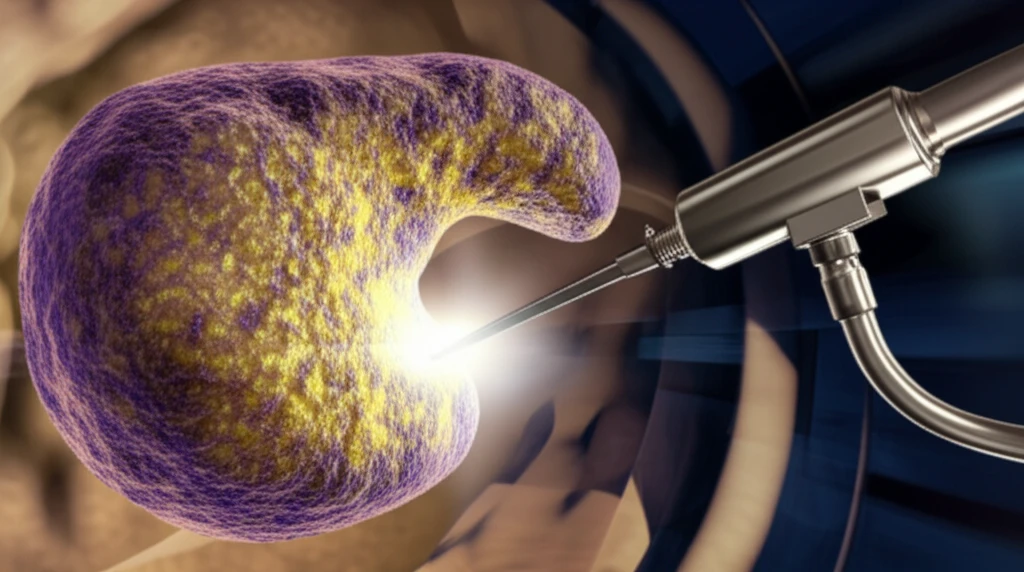
Staging laparoscopy involves inserting a thin, lighted tube with a camera into the abdomen to visually inspect the organs for signs of cancer spread. The procedure allows surgeons to identify small metastases that may not be detected by CT scans or MRIs. The argument for routine staging laparoscopy in LAPC stems from the desire to avoid unnecessary surgeries in patients who already have widespread disease.
- Invasiveness: Laparoscopy is an invasive procedure that carries risks such as bleeding, infection, and injury to internal organs.
- Cost: The procedure adds to the overall cost of cancer treatment.
- Delay: It can delay the start of potentially beneficial systemic therapies.
- Limited Impact on Survival: Some argue that even if micrometastases are detected and surgery is avoided, the overall survival benefit may be limited, as the cancer is likely to recur despite systemic treatment.
Moving Forward: The Need for More Evidence
The debate surrounding staging laparoscopy in LAPC highlights the need for more research to identify which patients benefit most from this procedure. As Drs. Paik and Kim note, the introduction of more effective chemotherapy regimens like FOLFIRINOX may change the landscape of neoadjuvant therapy and influence the role of surgical restaging. Ultimately, the decision of whether or not to perform staging laparoscopy should be made on a case-by-case basis, considering the individual patient's characteristics, the stage of their cancer, and the availability of effective systemic therapies.
