Optimizing Brachytherapy: How Bladder Volume Impacts Radiation Dose in Cervical Cancer Treatment
"A Deep Dive into Balancing Risk and Effectiveness in Intracavitary Brachytherapy for Cervical Cancer"
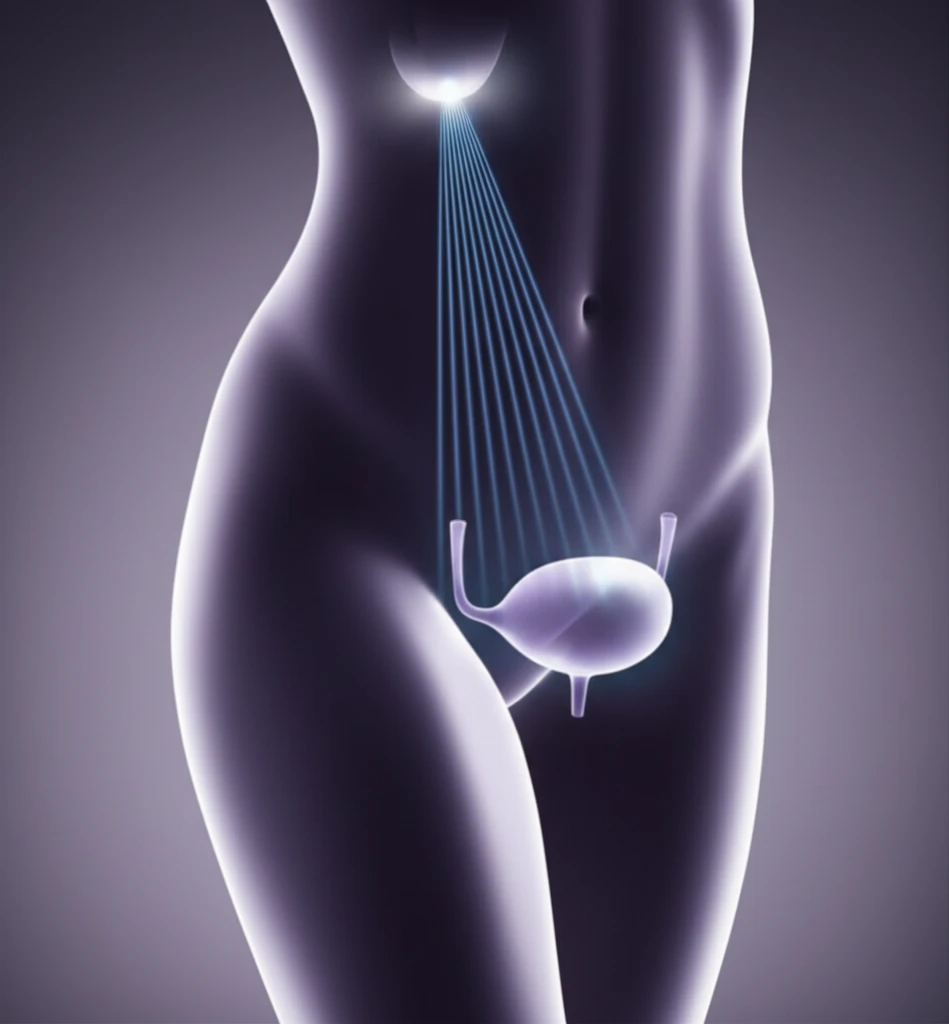
Cervical cancer treatment often involves a combination of external beam radiation therapy and brachytherapy, a procedure where radioactive sources are placed inside the body near the tumor. Intracavitary brachytherapy, specifically, is a common technique used to target cervical tumors, but it also poses a risk to nearby organs like the bladder, rectum, and small intestine.
Balancing the radiation dose to effectively kill cancer cells while minimizing damage to these organs is a critical challenge. Medical physicists and radiation oncologists use sophisticated planning techniques to optimize the dose distribution, and imaging plays a key role in this process. Recent research has focused on how the volume of the bladder during brachytherapy can impact the radiation dose received by these organs at risk.
This article explores the findings of a study investigating the effect of bladder volume on radiation dose distribution during intracavitary brachytherapy for cervical cancer. By understanding these effects, clinicians can refine their treatment planning strategies to improve patient outcomes and reduce the risk of complications.
Bladder Volume: A Key Factor in Radiation Dose Distribution
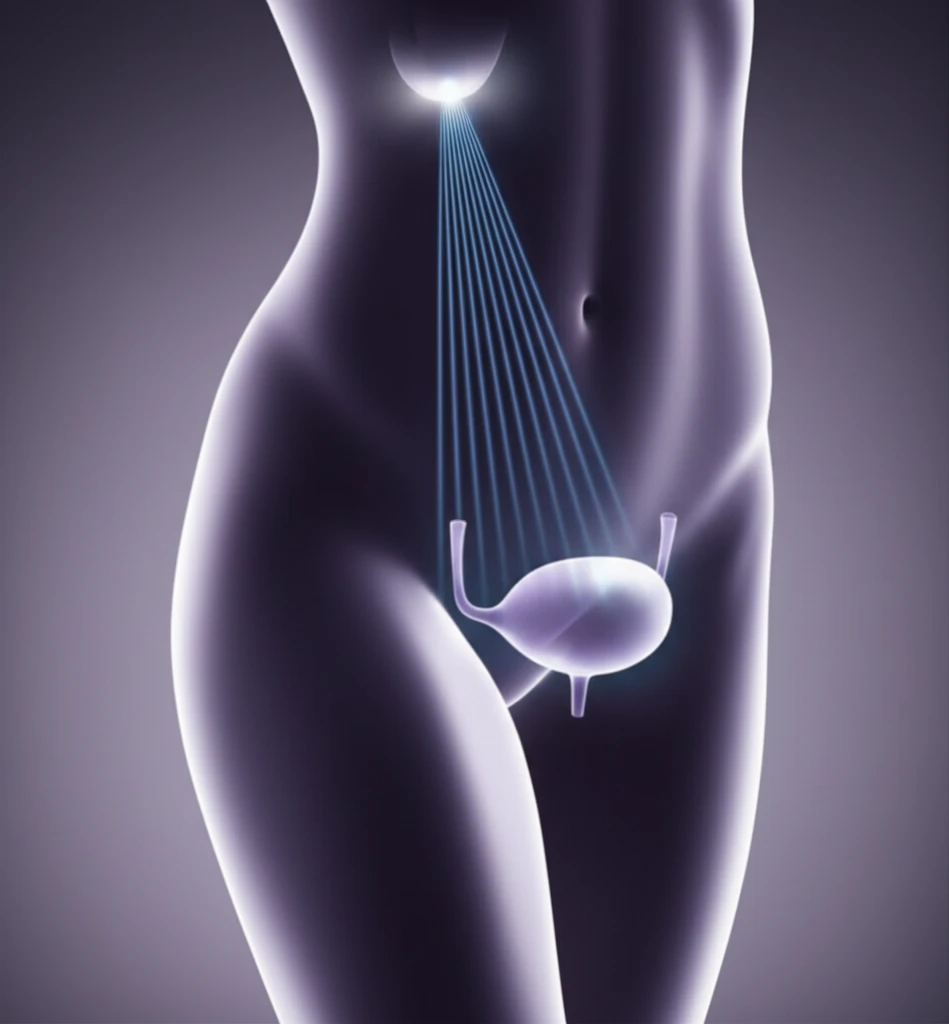
A prospective study was conducted involving 20 patients undergoing intracavitary brachytherapy for cervical cancer following external beam radiation. Each patient underwent two simulated dosimetries: one with a full bladder and one with an empty bladder. The goal was to assess how bladder volume affects the radiation dose received by the bladder itself, as well as the rectum and small intestine.
- Bladder Dose: The average D2cm³ to the bladder increased significantly, from 6.8 Gy with an empty bladder to 8.5 Gy with a full bladder. This corresponded to an increase from 83 Gy to 99 Gy in EQD2, a 16% increase.
- Small Intestine Dose: The average D2cm³ to the small intestine decreased significantly, from 4.75 Gy with an empty bladder to 2.61 Gy with a full bladder. This translates to a decrease from 62 Gy to 50 Gy EQD2.
- Rectal Dose: No significant difference was observed in the D2cm³ to the rectum based on bladder volume.
The Path Forward: Refining Brachytherapy Techniques
This research underscores the importance of carefully considering bladder volume during brachytherapy planning for cervical cancer. While the study suggests that an empty bladder may be preferable, further investigation is needed to fully understand the long-term clinical implications.
Future studies could explore the optimal bladder volume range, taking into account individual patient anatomy and tumor characteristics. Advanced imaging techniques and dose optimization algorithms could also be used to further refine treatment plans and minimize the risk of complications.
Ultimately, the goal is to deliver the most effective radiation dose to the tumor while sparing healthy tissues, leading to improved survival rates and quality of life for women undergoing brachytherapy for cervical cancer. This research is a step forward in achieving that goal.
