New Hope for Barrett's Esophagus: An Improved Surgical Model
"Scientists develop a more effective way to study and potentially treat this precursor to esophageal cancer."
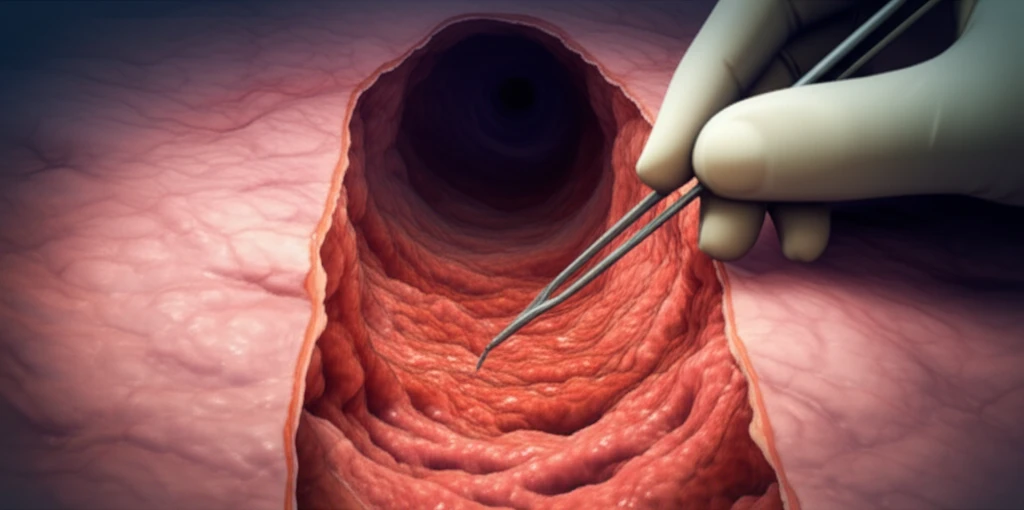
Barrett's esophagus (BE) is a serious condition where the lining of the esophagus changes, increasing the risk of esophageal adenocarcinoma. Current animal models used to study BE often have low success rates and require lengthy observation periods. This makes researching new treatments and understanding the disease's progression challenging.
Now, researchers have developed an improved surgical procedure that significantly increases the incidence of BE in rats. This breakthrough promises to accelerate research and provide a more reliable platform for testing potential therapies.
This article will explain the new surgical model, its advantages over previous methods, and its potential impact on the future of BE research and treatment.
The Breakthrough: A Modified Surgical Approach
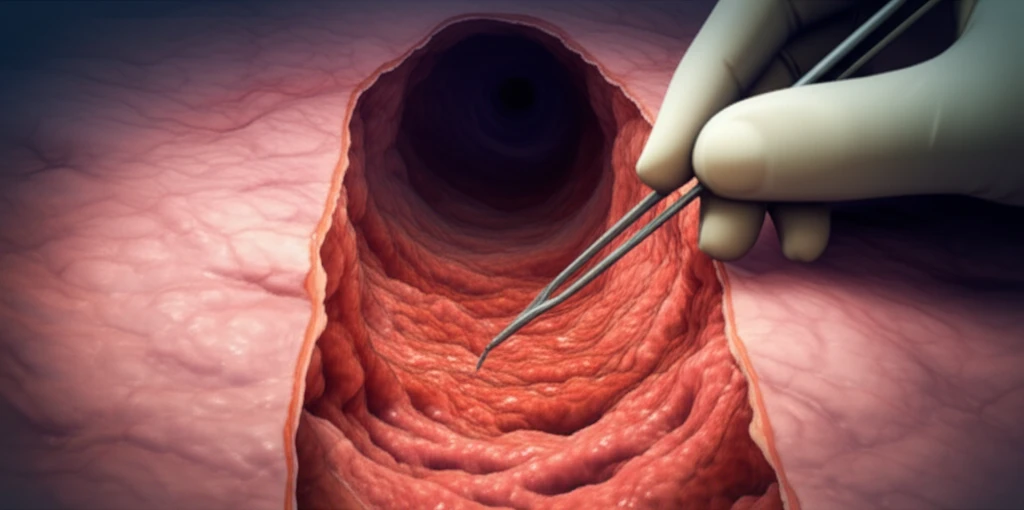
The researchers modified a previously existing surgical model (EJGJ) to create a more effective method for inducing BE in rats. The key modifications involved:
- Shortening the Distance: The distance between the Treitz ligament and the gastro-jejunal anastomosis was reduced to 3 cm.
- Lengthening the Distance: The distance between the stomach-jejunal anastomosis (SJA) and the esophagus-jejunal anastomosis (EJA) was increased to 1-1.5 cm.
Implications for Future Research
This improved surgical model represents a significant step forward in BE research. Its higher success rate and faster induction time will enable scientists to:
This research offers hope for more effective treatments and a better understanding of this complex disease. This model offers a reliable method for further investigation and potential therapeutic breakthroughs, ultimately benefiting patients at risk of esophageal cancer.
The team has continued to refine this technique, and future work will focus on reducing post-surgical complications to create a reliable tool for BE research.
