Navigating Postpartum Hemorrhage: A Guide to Understanding and Management
"From Prevention to Intervention: A Comprehensive Look at Postpartum Hemorrhage and the Steps Taken to Ensure Maternal Health."
The joy of welcoming a new life into the world can sometimes be overshadowed by unforeseen complications. Postpartum Hemorrhage (PPH), or excessive bleeding after childbirth, is one such challenge. It's a condition that demands immediate attention, as it can pose a significant risk to a mother's health. Understanding PPH, its causes, and the various approaches to its management is crucial for both medical professionals and expectant parents.
This article provides an in-depth exploration of PPH. We'll cover the factors that contribute to this condition, the steps taken to prevent it, and the range of treatments available when it occurs. Our aim is to offer a clear, reassuring guide, designed to empower readers with knowledge and foster a sense of preparedness.
We will explore the medical interventions, from initial assessments to advanced surgical techniques, all while emphasizing the importance of a timely, well-coordinated response. The information presented here is intended to be informative and supportive, reflecting the complexities of PPH while aiming to reduce anxiety and promote understanding.
Understanding Postpartum Hemorrhage: Causes and Risk Factors
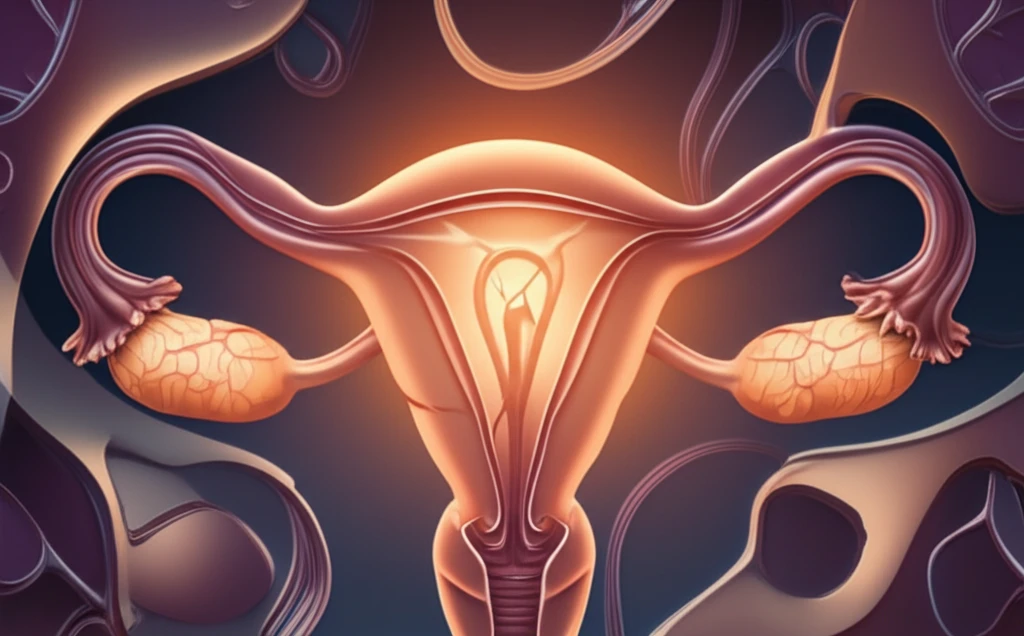
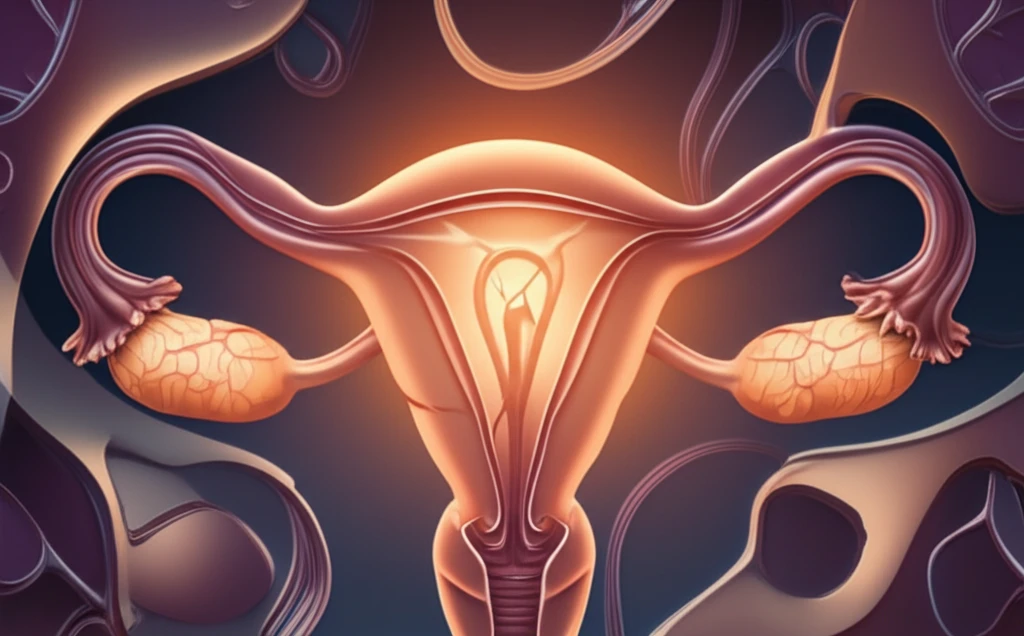
Postpartum hemorrhage is generally defined as the loss of a substantial amount of blood—typically more than 500 milliliters after a vaginal birth or more than 1,000 milliliters after a cesarean section. Several factors can lead to PPH, and often, a combination of these contributes to the condition. Understanding these causes is the first step in effective prevention and treatment.
- Tone: This refers to the uterine atony, or the failure of the uterus to contract adequately after delivery. This is the most common cause of PPH.
- Tissue: The retention of placental tissue within the uterus can prevent the uterus from contracting properly.
- Trauma: Lacerations, tears in the vaginal wall, cervix, or uterus, can cause significant bleeding.
- Thrombin: Blood clotting disorders or coagulopathies can impair the body's ability to form clots, leading to excessive bleeding.
Empowering Mothers and Supporting Healthy Outcomes
Postpartum Hemorrhage is a serious but manageable complication. By understanding the causes, recognizing the risk factors, and being aware of the available treatment options, both medical professionals and expectant parents can approach childbirth with greater confidence. This guide serves as a resource for promoting awareness and fostering a proactive approach to maternal health, ensuring the best possible outcomes for both mother and child.
