Navigating Postpartum Hemorrhage: A Comprehensive Guide to Surgical Management
"When medical interventions fall short, understanding surgical options can be crucial for maternal health and recovery."
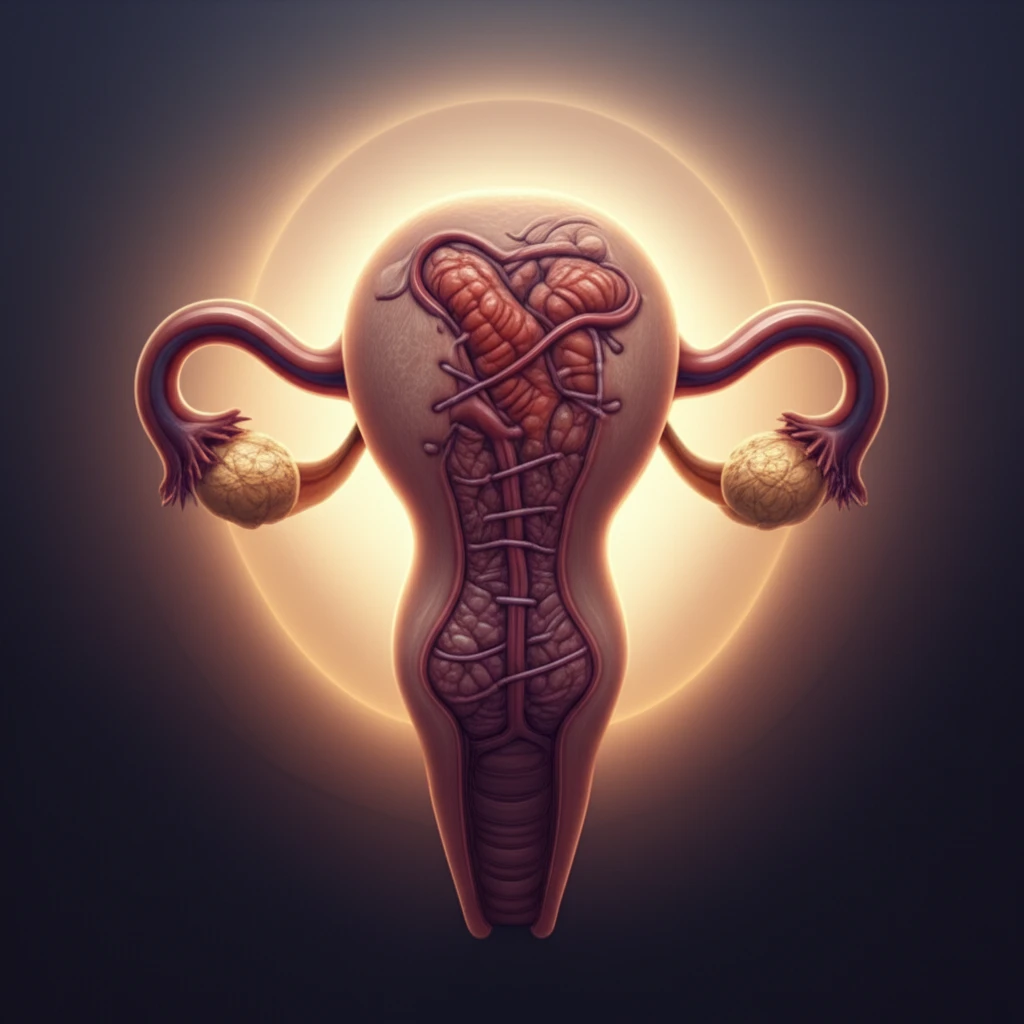
Postpartum hemorrhage (PPH), or excessive bleeding after childbirth, is a critical concern in maternal healthcare. While medical management is the first line of defense, surgical interventions become necessary when these methods prove insufficient. Knowing when and how to proceed with surgical options can significantly reduce maternal morbidity and mortality.
This guide addresses surgical strategies for PPH, emphasizing the importance of preparation, resource mobilization, and a systematic approach to evaluation and surgical management. We aim to provide clear insights into the various surgical techniques available, highlighting their roles in controlling PPH and preserving fertility where possible.
Although numerous conservative surgical approaches exist, it's crucial to recognize when definitive management, such as a hysterectomy, is necessary to protect a hemodynamically unstable patient. This guide will help healthcare providers make informed decisions, ensuring the best possible outcomes for mothers experiencing PPH.
Understanding the 4 T's of Postpartum Hemorrhage: A Guide to Evaluation and Management
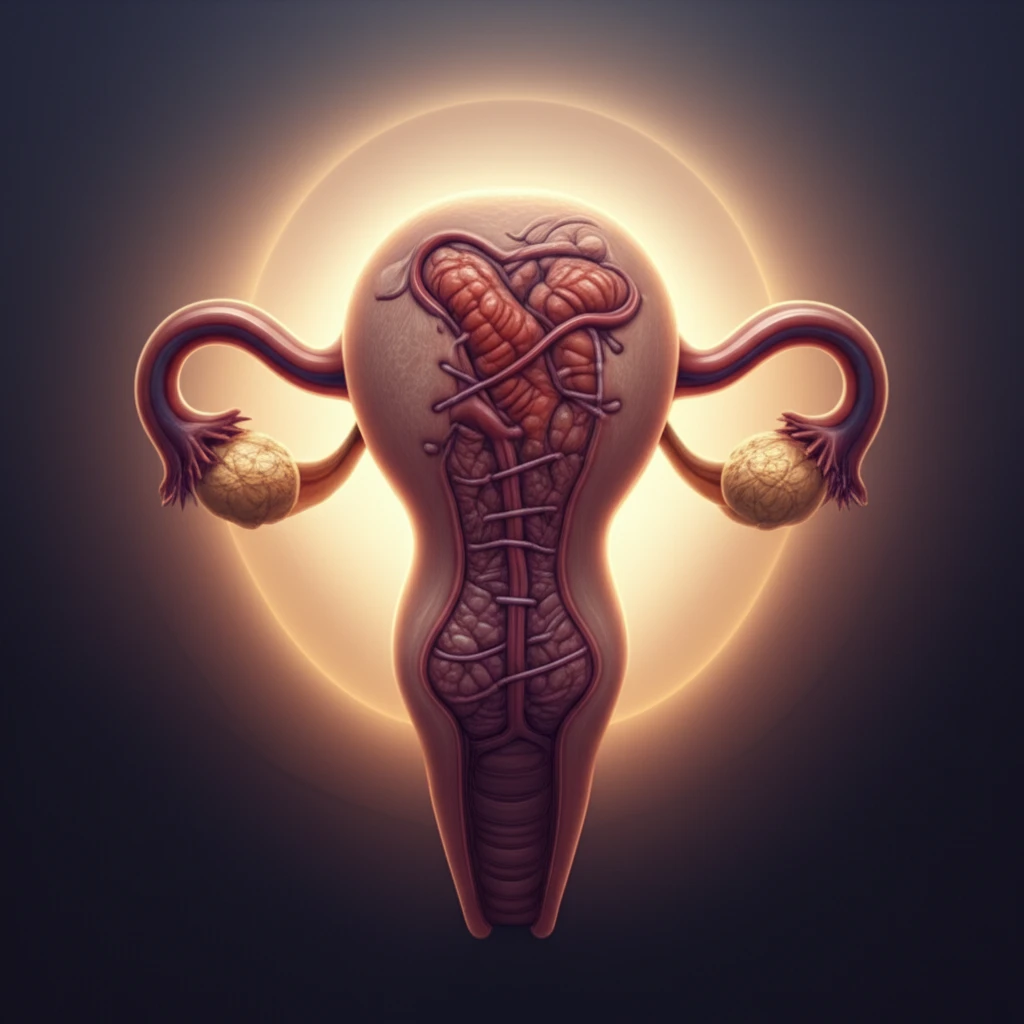
When tackling postpartum hemorrhage (PPH), it's helpful to think in terms of the "4 Ts": Tone, Trauma, Tissue, and Thrombin. Each 'T' represents a different cause of bleeding after childbirth, and understanding these causes is key to providing the right treatment. Surgical management focuses on improving uterine tone, removing any retained tissue, and repairing trauma, all while preventing further blood loss.
- Restoring Uterine Contractility: Techniques aimed at removing retained tissue and repairing any trauma to the uterus, helping it contract properly.
- Decreasing Blood Loss: Procedures designed to reduce blood flow to the uterus, giving the body time to restore its natural tone and prevent further bleeding.
- Providing "Tone" Through Tamponade: Methods using internal or external pressure to help the uterus contract and stop the bleeding.
The Importance of Readiness
Though various conservative, fertility-sparing surgical approaches can be used in the setting of PPH, in a hemodynamically unstable patient, team readiness for definitive management with a hysterectomy is necessary in order to reduce the risk of maternal mortality.
