Navigating Cystic Fibrosis as an Adult: A Comprehensive Guide to Acute Complications
"From respiratory distress to digestive dilemmas, learn how to manage acute health crises in adult cystic fibrosis patients for a better quality of life."
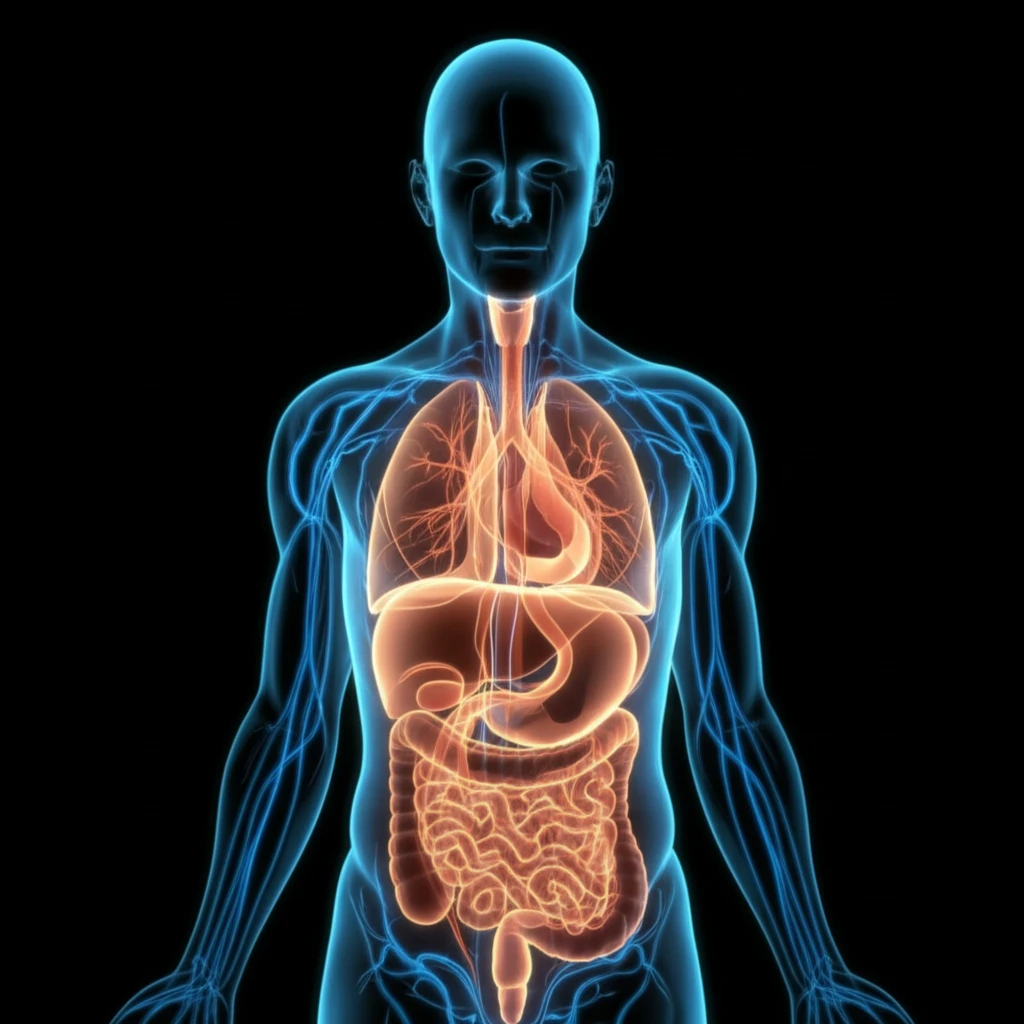
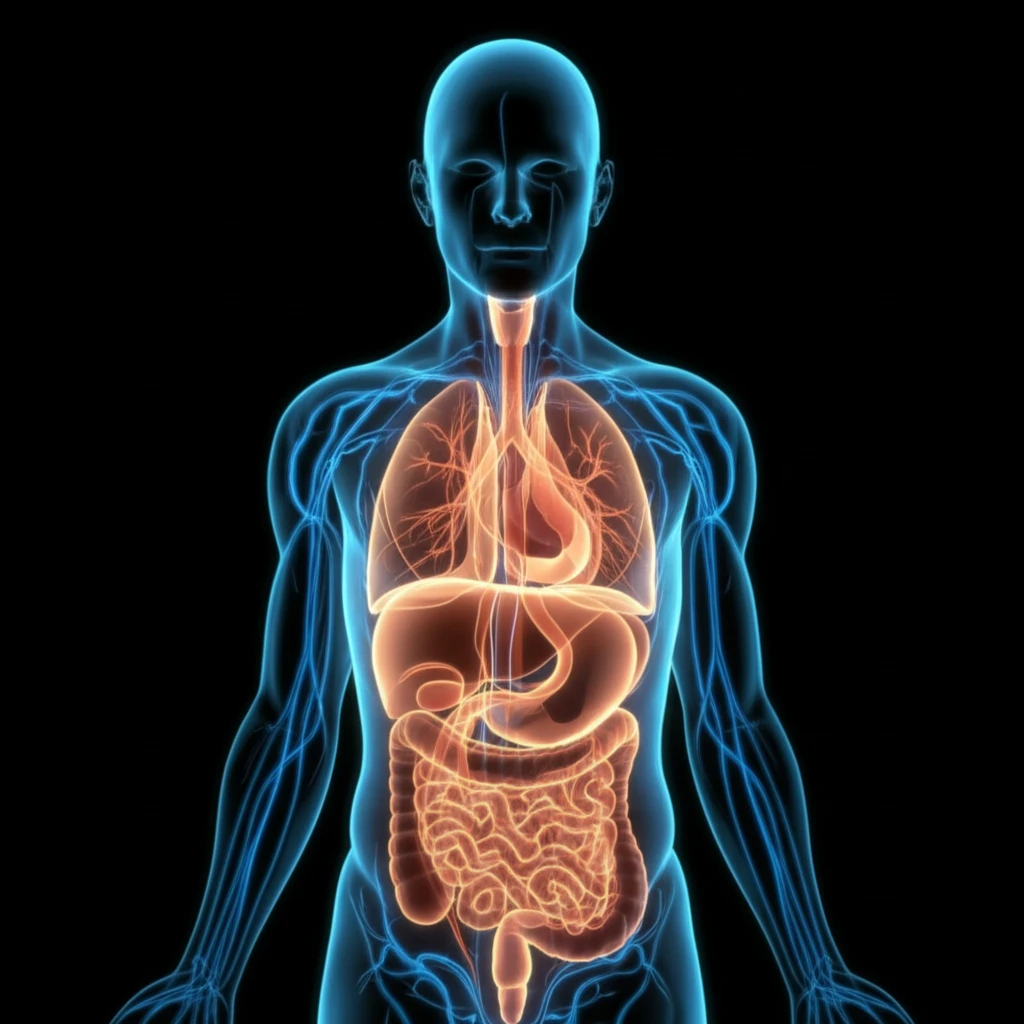
Cystic Fibrosis (CF) is a genetic disease primarily affecting the lungs and digestive system. It's caused by a defective gene that leads to a buildup of thick mucus in the body. This can lead to chronic respiratory infections, difficulty breathing, and problems with digestion. While often diagnosed in childhood, many individuals with CF are now living well into adulthood, thanks to advances in treatment and care.
However, adulthood brings its own set of challenges for people with CF. Acute complications—sudden and severe health issues—can arise, requiring prompt recognition and management. These complications can range from respiratory distress to digestive dilemmas, and may occur outside of specialized CF centers, making general medical knowledge crucial.
This guide focuses on providing comprehensive information about the acute complications adults with CF might face. We will explore key strategies for managing respiratory and non-respiratory emergencies, ensuring that patients and their caregivers are well-equipped to handle these challenges effectively.
Breathing Easy: Tackling Acute Respiratory Complications
Respiratory issues remain the leading cause of health problems for individuals with CF. The buildup of thick mucus in the lungs creates an environment ripe for bacterial infections and chronic inflammation. Let's break down some of the most common acute respiratory complications:
- Exacerbations: These are sudden flare-ups of respiratory symptoms, marked by increased coughing, mucus production, shortness of breath, and fatigue. They often result from bacterial infections. Treatment typically involves antibiotics (oral, inhaled, or intravenous), airway clearance techniques (like chest physiotherapy), and sometimes non-invasive ventilation.
- Hemoptysis: This refers to coughing up blood. While it can be alarming, mild hemoptysis is relatively common in CF. However, significant bleeding requires immediate medical attention. Treatment options range from antibiotics to address underlying infections to bronchial artery embolization (BAE) to stop the bleeding.
- Pneumothorax: This occurs when air leaks into the space between the lung and the chest wall, causing the lung to collapse. Symptoms include sudden chest pain and shortness of breath. Treatment may involve observation, needle aspiration, or chest tube insertion to remove the air.
- Allergic Bronchopulmonary Aspergillosis (ABPA): This is an allergic reaction to the fungus Aspergillus fumigatus, which can colonize the airways of people with CF. Symptoms include wheezing, coughing, fever, and mucus plugs. Treatment typically involves corticosteroids and antifungal medications.
Empowering Adults with CF: Taking Charge of Your Health
Living with cystic fibrosis as an adult requires proactive management and a collaborative approach with your healthcare team. By understanding the potential acute complications and knowing how to respond, you can empower yourself to live a healthier, more fulfilling life. Stay informed, stay connected, and remember that you're not alone in this journey.
