Mesh Materials for Genital Prolapse Repair: Which Type is Best?
"A comparison of synthetic and biosynthetic meshes reveals key differences in outcomes and complications after surgical treatment for severe genital prolapse."
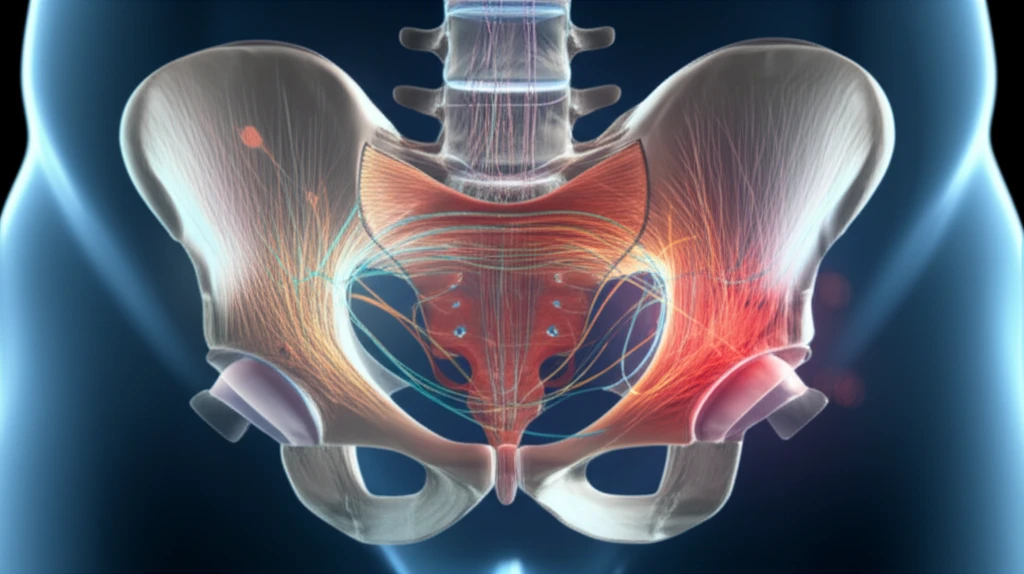
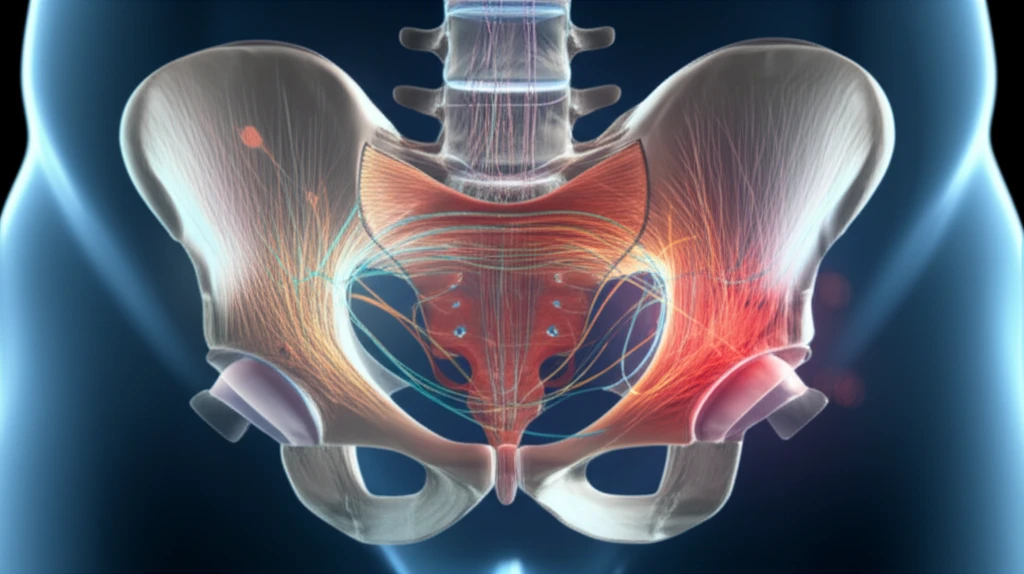
Genital prolapse significantly impacts women's quality of life, leading to discomfort, pain, and functional limitations. While synthetic meshes have revolutionized surgical repair, offering excellent anatomical restoration, the risk of erosion remains a concern. This has led to the exploration and development of biosynthetic meshes as alternatives.
Both synthetic and biosynthetic meshes aim to provide structural support to weakened pelvic tissues. However, they differ significantly in their composition and properties. Synthetic meshes are typically made of polypropylene, a durable but non-absorbable material. Biosynthetic meshes, on the other hand, incorporate biological components like collagen, which are designed to promote tissue integration and potentially reduce erosion risk.
This article explores a study comparing the effectiveness and safety of two surgical procedures using different mesh types: the Prolift™ system (synthetic) and the Avaulta™/Avaulta Plus™ system (biosynthetic). We'll delve into the findings, highlighting the benefits and drawbacks of each approach to help you understand the factors influencing surgical outcomes and potential complications.
Synthetic vs. Biosynthetic Mesh: Understanding the Key Differences
The study retrospectively analyzed data from 158 women with severe genital prolapse (stages III-IV POP-Q). Eighty-six patients received the Prolift™ system with a synthetic polypropylene mesh (Group A), while seventy-two underwent surgery with the Avaulta™/Avaulta Plus™ system, utilizing a biosynthetic polypropylene mesh coated with porcine collagen (Group B).
- Anatomical Outcomes: Both groups showed significant improvement in anatomical support. The objective cure rate was 89.5% in the synthetic mesh group (A) and 86.1% in the biosynthetic mesh group (B).
- Erosion Rates: Mesh exposure occurred in 8.1% of patients in group A (synthetic) and 5.6% in group B (biosynthetic).
- Functional Outcomes: Both groups reported improvements in dyspareunia (painful intercourse) and overactive bladder symptoms.
- Quality of Life: Significant improvements were observed in both groups based on VAS questionnaires for prolapse, UDI-6 s.f., the IIQ7 s.f. and the PISQ-12 scores.
Making Informed Decisions About Prolapse Repair
The decision of whether to use synthetic or biosynthetic mesh for genital prolapse repair should be made in consultation with a qualified surgeon. Factors to consider include the severity of the prolapse, patient-specific risk factors, and individual preferences.
While biosynthetic meshes show promise in reducing erosion risk, long-term data is still needed to fully evaluate their durability and effectiveness compared to synthetic meshes. Ongoing research continues to refine surgical techniques and improve mesh materials, aiming to optimize outcomes and minimize complications for women undergoing prolapse repair.
Ultimately, a thorough discussion with your healthcare provider is crucial to determine the most appropriate surgical approach and mesh type for your individual needs, ensuring the best possible outcome and improved quality of life.
