Meloxicam and Your Gut: What You Need to Know About NSAID-Induced Intestinal Issues
"A deep dive into the risks of GI bleeding and stenosis linked to meloxicam, empowering you to make informed decisions about your health and pain management."
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a common class of medications used to manage pain and inflammation. Among these, meloxicam, a COX-2 selective NSAID, is frequently prescribed for conditions like arthritis and chronic back pain. While generally considered safer for the stomach than traditional NSAIDs, recent reports suggest that meloxicam is not without its risks.
A case report published in Reactions detailed a concerning instance of a 72-year-old man who developed severe gastrointestinal (GI) issues after prolonged use of meloxicam. This case highlights the potential for meloxicam to cause serious complications, including GI bleeding and multiple stenoses (narrowing) in the small intestine.
This article aims to break down the details of this case report, explain the potential risks associated with meloxicam, and provide you with information on how to protect your gut health while managing pain. We will explore the underlying mechanisms, symptoms to watch out for, and alternative strategies for pain relief.
Understanding the Case: Meloxicam's Impact on the Small Intestine
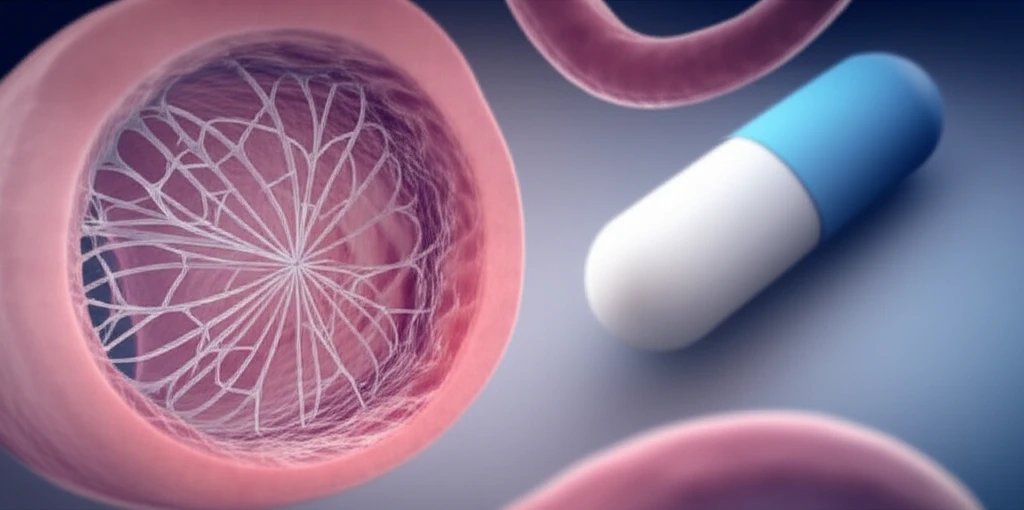
The 72-year-old patient in the case report had been taking 300 mg of oral meloxicam daily for two years to manage chronic back pain. He began experiencing abdominal fullness, unexplained gastrointestinal bleeding, and recurrent small intestinal ileus (blockage). These symptoms prompted hospitalization and further investigation.
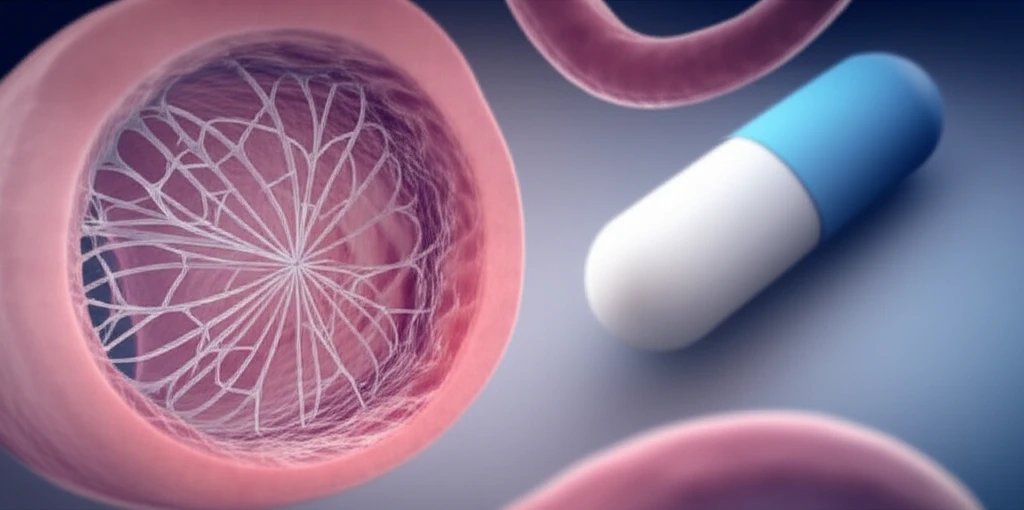
- Pinhole membranous stenoses: Multiple tiny, web-like constrictions in the mid-jejunum (a section of the small intestine).
- Ulcer scars: Evidence of previous damage and inflammation in the small intestine.
- Microscopic changes: Tissue samples showed abnormalities, including reduction of the cervical region in the epithelium, sub-epithelial fibrosis, collagen hyperplasia, and changes in pericryptal cells to myofibroblasts. Apoptotic bodies (cells undergoing programmed death) were also observed.
Protecting Your Gut: Alternative Strategies and Precautions
The case report serves as a reminder of the potential risks associated with even COX-2 selective NSAIDs like meloxicam. While these medications can be effective for pain management, it's crucial to be aware of the potential side effects and take proactive steps to protect your gut health. If you are taking meloxicam or another NSAID, talk to your doctor about strategies to minimize your risk of GI complications. This may include exploring alternative pain management options, using the lowest effective dose of NSAIDs, and considering concomitant use of gastroprotective medications.
