Mastering Anastomotic Leaks: A Proactive Guide for Colonic Resection
"Expert insights and practical strategies to prevent and manage anastomotic leaks, ensuring safer outcomes in colon surgery."
Anastomotic leaks represent one of the most formidable challenges in colon and rectal surgery. These complications, if not promptly recognized and appropriately managed, can lead to severe septic conditions and potentially fatal outcomes. The review by Drs. Tutone and Hill serves as a critical resource for surgeons, providing a comprehensive overview of the presentation, diagnosis, and management of anastomotic leaks following colectomy.
While the original article effectively outlines several preoperative, intraoperative, and postoperative risk factors, this discussion aims to expand on these points and incorporate additional clinical insights. By focusing on modifiable risk factors and emphasizing meticulous surgical techniques, the goal is to enhance patient safety and improve surgical outcomes.
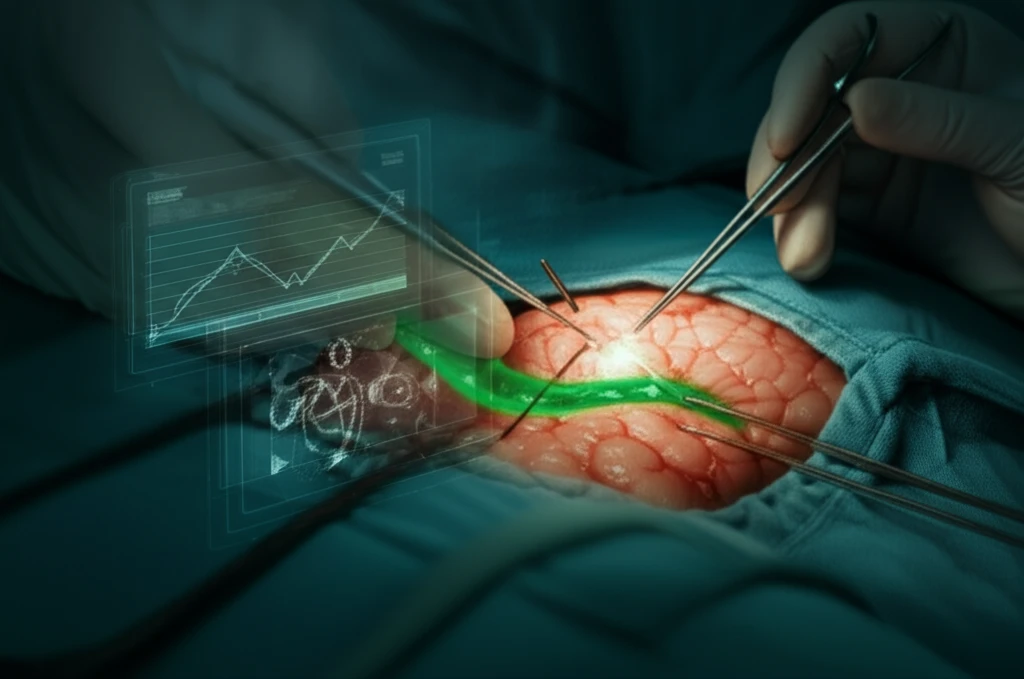
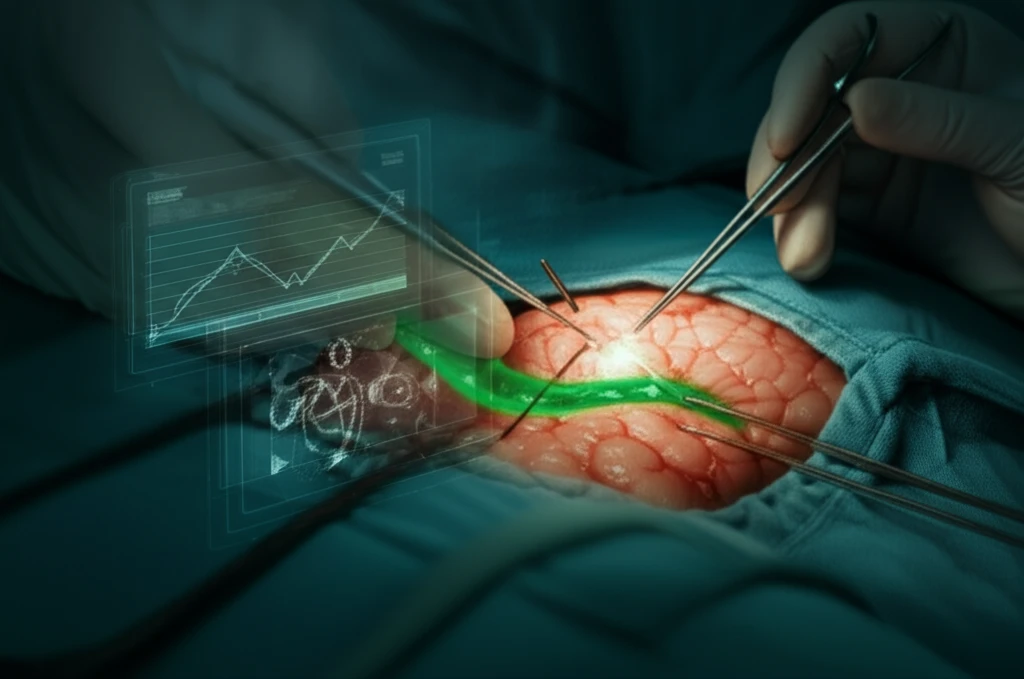
This commentary delves deeper into the optimization of patients before surgery, highlights the importance of nutritional status and immune function, and underscores the significance of mechanical bowel preparation. Additionally, it addresses intraoperative strategies, such as tension-free anastomosis and the judicious use of indocyanine green dye, to minimize the risk of leaks. Finally, it provides guidance on postoperative management, emphasizing the need for vigilant monitoring and prompt intervention when leaks are suspected.
Preoperative Optimization: Setting the Stage for Success
Several modifiable risk factors can be addressed preoperatively to significantly reduce the likelihood of anastomotic leaks. While cancer patients require timely intervention, other colorectal procedures can often be postponed to allow for comprehensive patient optimization. Key among these factors are nutritional status and immune function, both of which play critical roles in tissue healing and anastomotic integrity.
- Assess Nutritional Status: Measure albumin, prealbumin, and transferrin levels.
- Evaluate Sarcopenia: Use CT scans to assess muscle mass.
- Optimize Nutrition: Employ TPN or tube feeds to correct deficiencies.
- Control Diabetes: Refer patients with uncontrolled diabetes for endocrinology consults.
- Consider Bariatric Surgery: For morbidly obese patients, consider sleeve gastrectomy before colon resection.
Intraoperative Excellence and Postoperative Vigilance
Adhering to fundamental principles during surgery is crucial to minimize the risk of anastomotic leaks. A tension-free anastomosis is paramount, often requiring mobilization of the splenic flexure in sigmoid colectomies. For transverse colectomies, options include mobilizing both hepatic and splenic flexures or performing an extended right hemicolectomy. Reinforcing the stress points of the anastomosis with additional sutures and ensuring adequate blood supply by preserving the marginal artery are also critical steps.
