Lungs: The Unsung Heroes in Heart Failure?
"New research reveals the surprising role of lungs in producing a key heart failure marker, opening doors to novel treatment strategies."
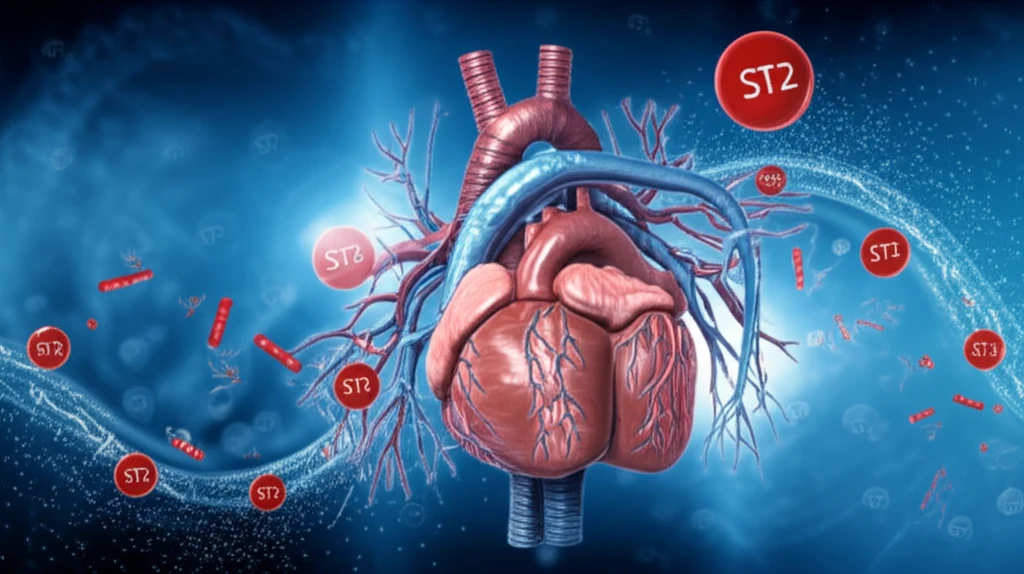
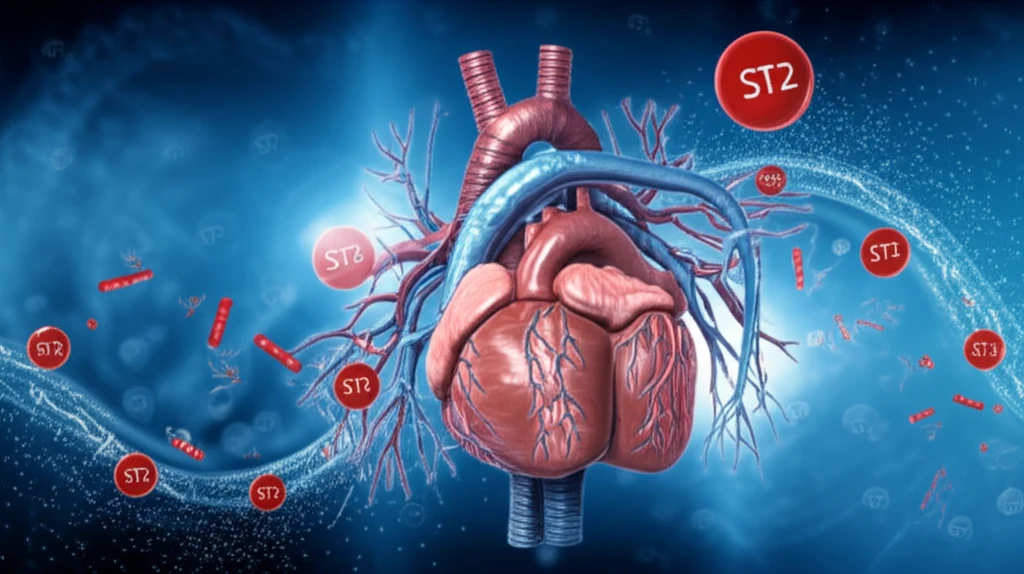
Heart failure, a condition where the heart struggles to pump enough blood to meet the body's needs, is a leading cause of disability and death worldwide. Scientists are constantly seeking new ways to understand and combat this complex disease. One area of intense research focuses on a molecule called ST2 (interleukin-1 receptor-like 1), a known prognostic marker in heart conditions.
While traditionally linked to the heart, recent evidence suggests that ST2 production might extend beyond the heart itself. This raises an important question: Could other organs be contributing to the levels of ST2 in the body, and if so, what impact might that have on heart failure?
New research has pinpointed the lungs as a significant, previously underestimated source of ST2 in heart failure. This discovery challenges existing views of the disease and opens exciting new avenues for developing targeted therapies to improve outcomes for patients.
How Lungs Contribute to Heart Failure: The ST2 Connection
The study, published in Circulation: Heart Failure, used an experimental model of ischemic heart failure to investigate ST2 production in various organs. Researchers measured ST2, its membrane-bound form (ST2L), and a related molecule called IL-33 in the lungs, heart, kidneys, and liver at different stages of heart failure. They also examined lung tissue and cells from patients with and without heart failure.
- Lungs step up: In the experimental model, ST2 levels increased significantly in the lungs early in heart failure.
- Heart's response: While ST2 also increased in the heart, the related molecules ST2L and IL-33 responded differently in the lungs and heart, suggesting distinct regulatory mechanisms.
- Lung cells pitch in: ST2 was found to be produced by type II pneumocytes, specialized cells in the lungs responsible for gas exchange. When these cells were subjected to mechanical strain (simulating the stress of fluid buildup in the lungs during heart failure), they released even more ST2.
- Human connection: Analyzing lung fluid from patients with cardiogenic pulmonary edema (fluid buildup in the lungs due to heart failure), researchers found significantly higher ST2 levels compared to patients with lung problems from other causes.
What This Means for Heart Failure Treatment
This research suggests that the lungs are not merely passive bystanders in heart failure but active participants in the disease process. By identifying the lungs as a significant source of ST2, scientists gain a deeper understanding of the complex interplay between the heart and other organs in heart failure.
This knowledge could lead to the development of new therapies specifically targeting ST2 production in the lungs. By reducing ST2 levels in the lungs, it might be possible to interrupt the harmful signaling pathways that contribute to heart failure progression and improve patient outcomes.
Future research will need to explore the precise mechanisms by which the lungs produce ST2 in heart failure and how this production contributes to overall disease severity. However, this study provides a compelling case for considering the lungs as a key player in heart failure and a potential target for future therapies.
