Lung Metastasectomy: How Size and Margins Can Improve Outcomes
"Understanding the factors beyond size and margin in lung metastasis resection for better prognosis."
The surgical removal of lung metastases is a topic of considerable debate within oncological and thoracic surgery circles. A central question persists: Does surgical resection truly enhance survival rates, or is the observed success simply a result of patient selection? Currently, concrete randomized evidence is lacking as we await the results from ongoing clinical trials.
The largest retrospective studies, encompassing over 5,000 patients and published in 1997, have pinpointed key factors influencing outcomes. Macroscopic complete resection, the number of metastases (with solitary metastases showing the best prognosis), and the disease-free interval all play crucial roles in predicting survival following surgery.
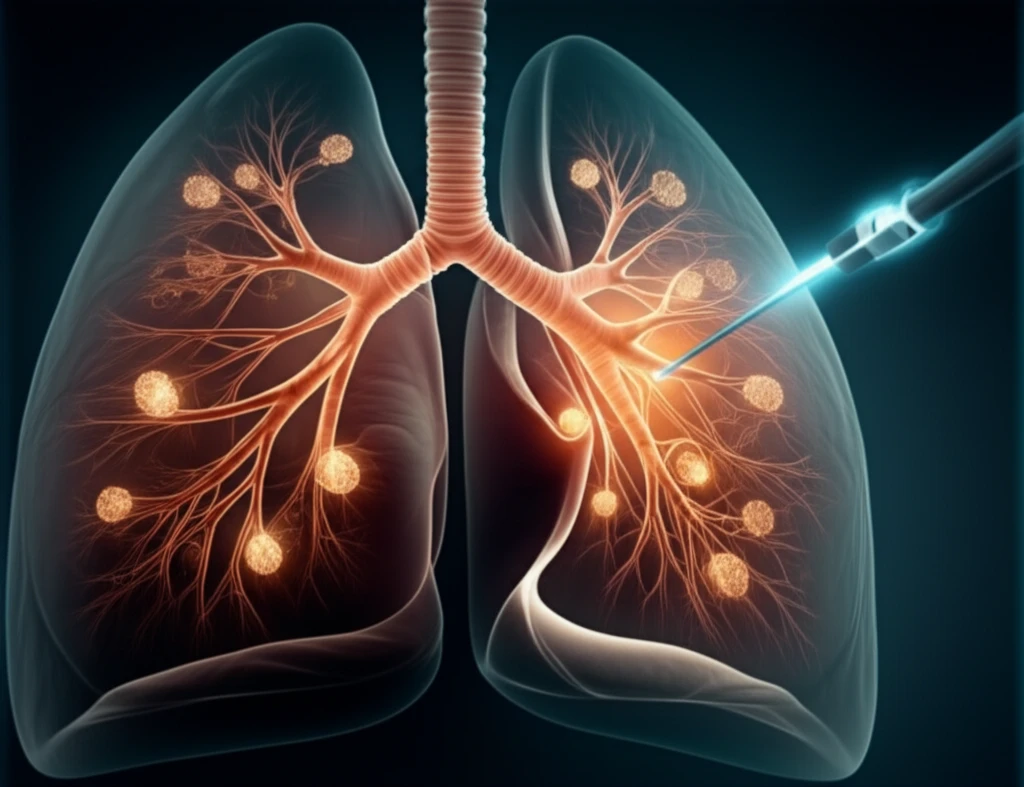
Unlike bronchogenic carcinoma, lung metastases are blood borne, and various surgical techniques have been refined to preserve lung tissue during removal. These methods range from clamping and suturing to laser ablation. Yet, establishing a definitive safe margin around these lesions remains an ongoing challenge.
What Margin Size Is Sufficient for Safe Lung Metastasectomy?
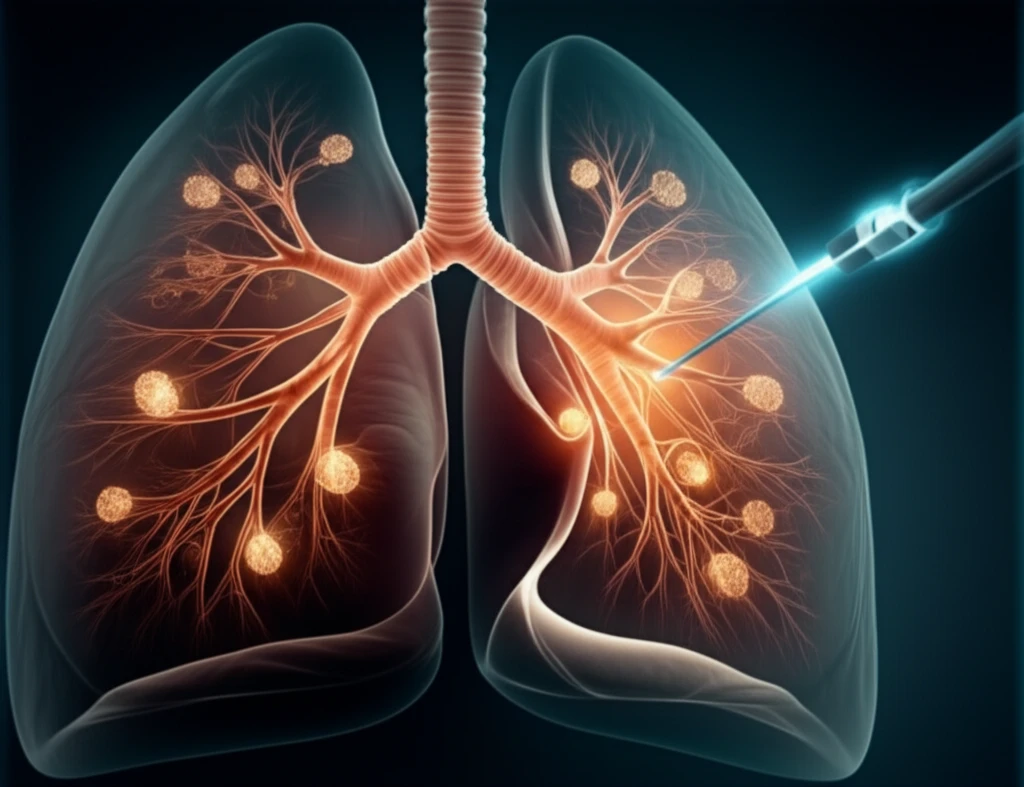
A recent study involving 335 patients who underwent 679 wedge resections for colorectal lung metastases revealed a 20.6% five-year risk of local recurrence. The research identified two significant factors: increasing the margin length decreased recurrence risk, whereas larger tumor size increased it. A margin length at least half the tumor size was deemed safe, reducing local recurrence to below 11%.
- Complete Resection: Macroscopic complete resection is critical for improved survival.
- Number of Metastases: Patients with a single metastasis typically have the best prognosis.
- Disease-Free Interval: A longer disease-free interval before metastasis indicates a better prognosis.
- Margin Length: A margin length at least half the tumor size is associated with lower local recurrence rates.
- Tumor Size: Smaller tumor sizes are correlated with decreased risk of recurrence.
Future Directions and the Oligometastatic Concept
Pulmonary metastatic disease will continue to be a focal point of research. The present study offers a timely contribution, indicating that maintaining a margin length of at least half the tumor size can indeed minimize the risk of recurrence. Further investigation and collaborative efforts are essential to refine treatment strategies and improve outcomes for patients with lung metastases.
