Lung Cancer Blood Flow: What Your Doctor Needs to Know
"New research unveils how different types of lung cancer—squamous cell carcinoma and adenocarcinoma—show unique blood flow patterns, potentially transforming treatment strategies."
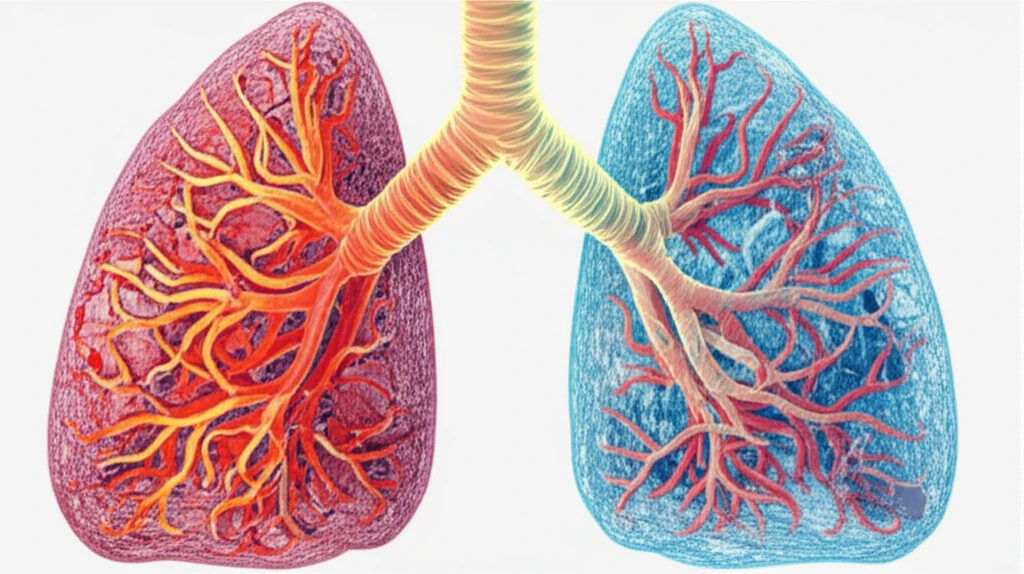
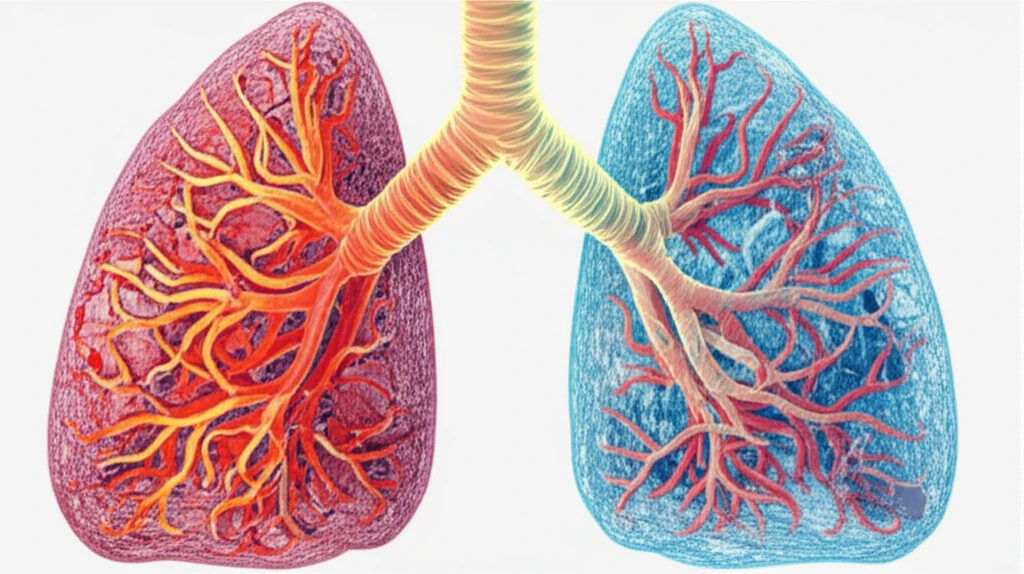
Angiogenesis, the creation of new blood vessels, is vital for tumor growth. By studying these vascular patterns, doctors can better understand and characterize different tissues. CT perfusion (CTp) is a promising technology that provides high-resolution spatial and temporal data, which helps in computing perfusion parameters by analyzing time-concentration curves (TCCs). These curves are generated as a contrast agent reaches the tumor, offering insights into its blood supply.
One of the most valuable perfusion parameters for evaluating angiogenesis is blood flow (BF). BF has a strong correlation with microvessel density (MVD), a key tissue biomarker. Measuring BF involves tracking the initial passage of a contrast medium, allowing for quick examinations that minimize radiation exposure. Clinically, BF information obtained at diagnosis can help characterize lesions, particularly in patients who are not eligible for surgery but need non-surgical treatments. Higher baseline BF values in advanced lung cancer patients may also indicate a better response to specific therapies.
Differences in BF values between patients who respond to treatment and those who do not have spurred interest in characterizing tumors based on their hemodynamic properties, including their histological subtypes. Characterizing non-small cell lung cancer (NSCLC) perfusion can provide valuable insights into a tumor's status, especially regarding its hypoxia (oxygen deficiency). Adenocarcinoma (AC), for instance, typically has a lower degree of hypoxia compared to squamous cell carcinoma (SCC). By understanding these differences, treatments can be tailored to improve outcomes.
Decoding Blood Flow in Lung Cancer: Adenocarcinoma vs. Squamous Cell Carcinoma
A recent study aimed to evaluate the distinct characteristics of lung tumors at diagnosis, focusing on potential differences in perfusion between adenocarcinoma (AC) and squamous cell carcinoma (SCC), the two most common NSCLC phenotypes. Previous research has presented conflicting results in AC and SCC perfusion characterization due to high measurement variability from clinical, physiological, and external factors (like patient movement and artifacts). To mitigate this variability, the study used an automatic method to detect and remove unreliable perfusion values.
- Study Design: The study involved 26 patients with primary NSCLC (19 AC and 7 SCC) who underwent CT perfusion at diagnosis.
- Data Collection: BF values were computed using the maximum-slope method, and unreliable values (e.g., those arising from artifacts or vessels) were automatically removed.
- Statistical Analysis: A one-tail Welch’s t-test was used to assess statistical significance, with a p-value < 0.05 indicating significance.
Future Implications for Lung Cancer Treatment
This research underscores the importance of understanding the unique blood flow characteristics of different lung cancer subtypes. By using CT perfusion to identify these patterns, doctors can make more informed decisions about treatment strategies, especially regarding antiangiogenic therapies for adenocarcinoma. Further studies are needed to explore these findings in larger patient cohorts and to investigate additional factors that may influence perfusion values. The ability to accurately profile tumors based on their perfusion characteristics holds great promise for personalized medicine in lung cancer treatment.
