Leg Saved: How a Dual Approach Conquered a Life-Threatening Blood Clot
"Discover how a cutting-edge combination of catheter-directed thrombolysis (CDT) and factor Xa inhibitors is changing the game for inferior vena cava (IVC) thrombosis treatment."
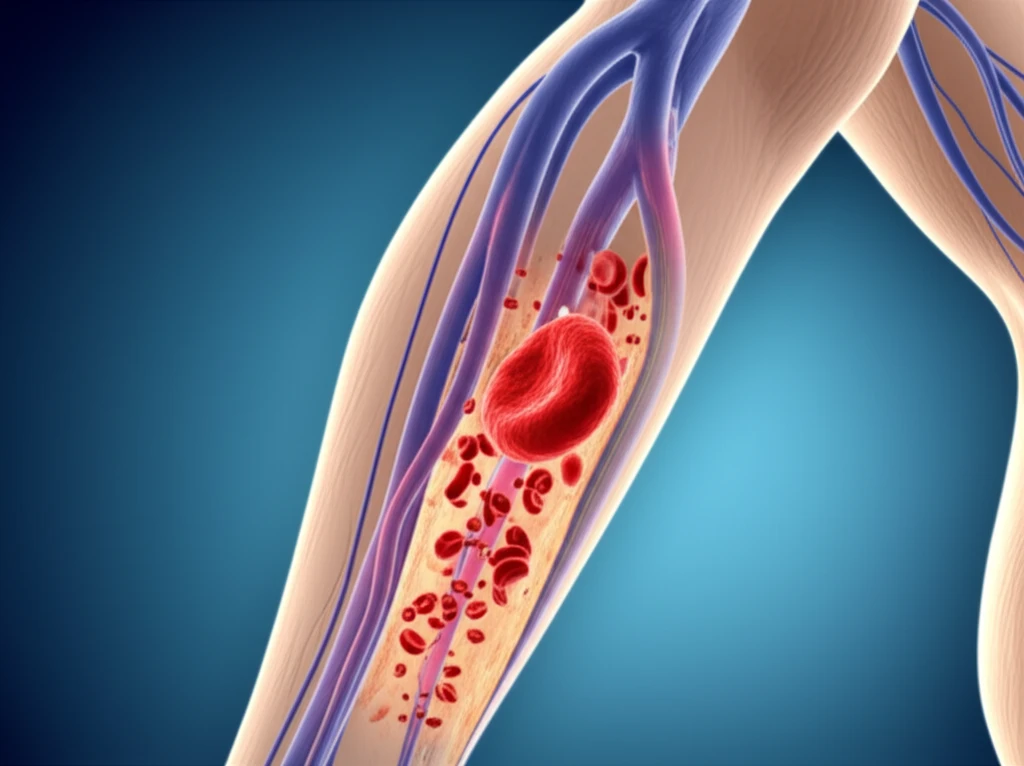
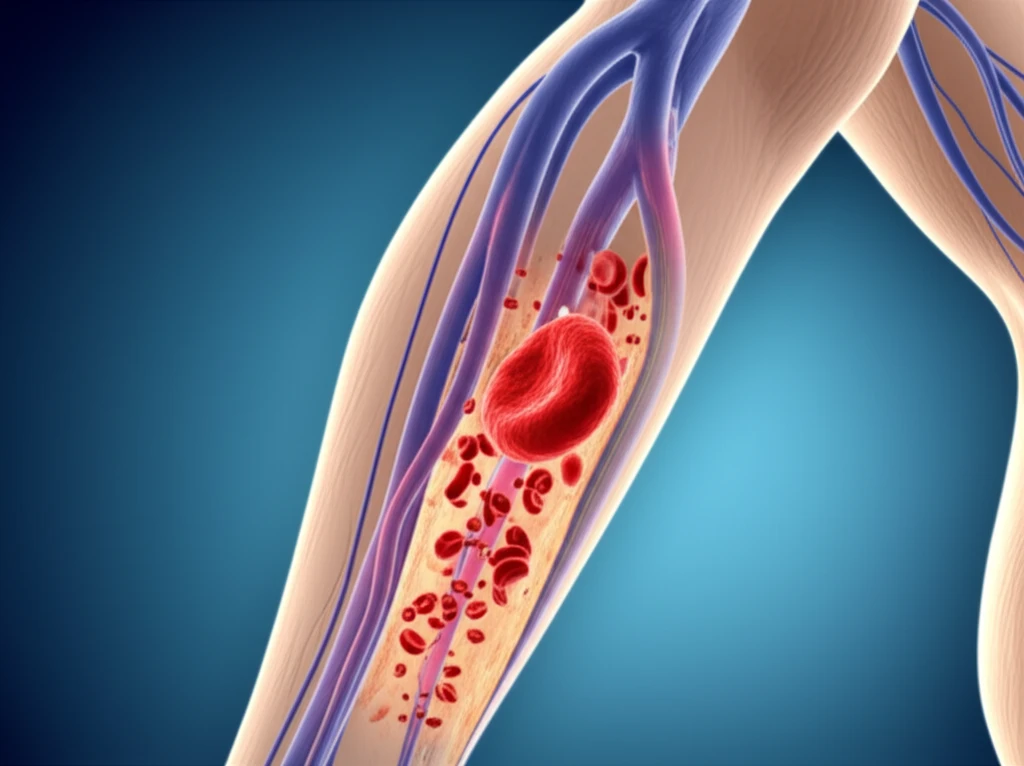
Venous thromboembolism (VTE), encompassing deep venous thrombosis (DVT) and pulmonary embolism (PE), poses a significant health risk. While DVT is a common cardiovascular issue, a massive clot extending into the inferior vena cava (IVC) is a rarer, more perilous condition.
When faced with extensive thrombosis carrying a high risk of pulmonary embolism (PE), interventional treatment becomes crucial. The combination of catheter-directed thrombolysis (CDT) and factor Xa inhibitors represents a powerful approach to not only dissolve the clot but also prevent long-term complications.
This article explores a compelling case where the integration of CDT and a factor Xa inhibitor effectively resolved a life-threatening situation. The combination offers new hope for patients facing similar challenges. The case highlights the transformative impact of advanced medical interventions in treating complex vascular conditions.
The Case: A Race Against the Clock
A 70-year-old man sought medical help due to severe symptoms in his left leg, including warmth, pain, swelling, and difficulty walking. His medical history included bronchial asthma, steroid-induced diabetes mellitus, eosinophilic sinusitis, eosinophilic pneumonia, and cerebral infarction. Physical examination revealed significant swelling and tenderness in the affected leg, with the left thigh circumference notably larger than the right.
- Initial Treatment with Fondaparinux: Subcutaneous fondaparinux, an anticoagulant, was administered. A Günther Tulip Filter was placed in the IVC to prevent the PE.
- Catheter-Directed Thrombolysis (CDT): After a week, with limited improvement from fondaparinux alone, CDT was initiated. A Fountain infusion catheter was advanced into the thrombus, delivering urokinase directly to dissolve the clot.
- Transition to Factor Xa Inhibitor: Following CDT, the treatment was switched to edoxaban, a direct oral anticoagulant (DOAC). This approach aimed to maintain the progress achieved by CDT and prevent recurrence.
A New Era in Thrombosis Treatment
The successful outcome in this case underscores the potential of combining CDT with factor Xa inhibitors for managing extensive DVT. This approach offers a targeted, effective way to dissolve clots and prevent complications, paving the way for improved outcomes and quality of life for patients facing these challenging conditions. The synergistic use of these therapies marks a significant advancement in the treatment of severe venous thromboembolism.
