Knee Pain Unlocked: Mastering Your Posteromedial Corner Health
"A Comprehensive Guide to Understanding, Treating, and Preventing Posteromedial Knee Injuries"
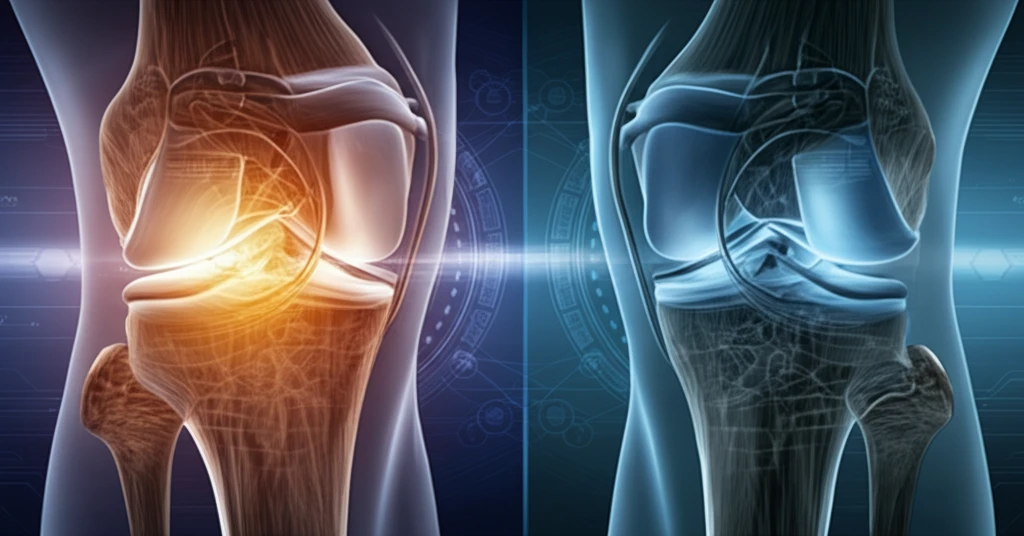
Knee pain can be a real game-changer, sidelining you from activities you love and impacting your day-to-day life. While many types of knee issues exist, one area often overlooked is the posteromedial corner (PMC). The PMC is a complex area on the inner side of your knee that's crucial for stability. When it's injured, it can lead to significant problems.
Think of the PMC as the unsung hero of your knee. It's made up of several key structures, including ligaments and tendons, that work together to keep your knee stable, especially during twisting and turning movements. Understanding the PMC and how injuries occur is the first step in protecting your knee health.
This guide aims to shed light on the PMC, providing you with the knowledge to understand, manage, and prevent injuries in this critical area of your knee. We'll break down the anatomy, common injuries, treatment options, and practical tips to keep your knees healthy and strong.
Decoding the Posteromedial Corner: Anatomy and Common Injuries
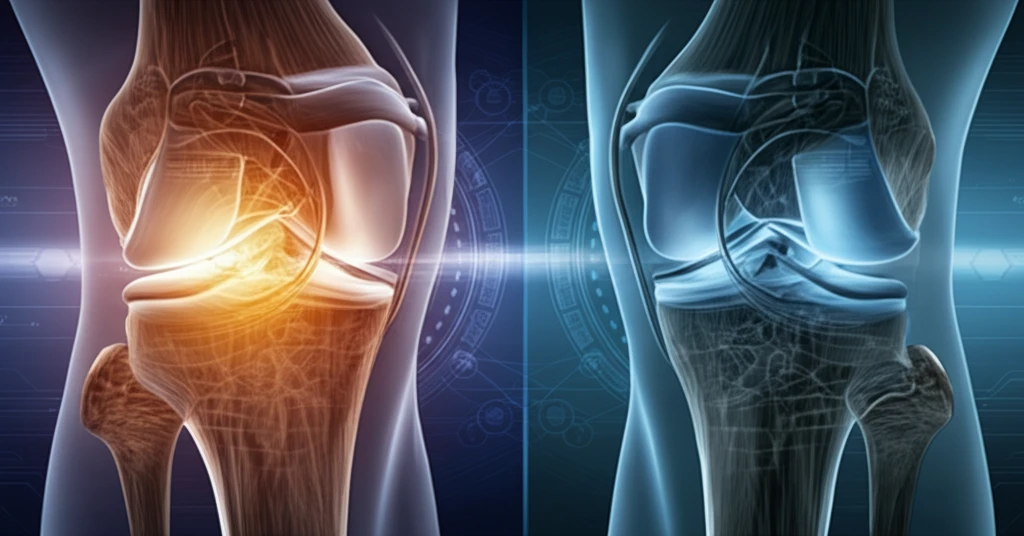
The posteromedial corner isn't just one thing; it's a team of structures working together. Key players include the superficial medial collateral ligament (MCL), the posterior oblique ligament (POL), parts of the semimembranosus tendon, the joint capsule, and even the medial meniscus. These structures provide stability against valgus stress (force pushing the knee inward) and control rotation.
- MCL Sprains: Stretching or tearing of the medial collateral ligament.
- POL Injuries: Damage to the posterior oblique ligament, which can lead to rotatory instability.
- Meniscal Tears: Tears in the medial meniscus, often occurring with other PMC injuries.
- Avulsion Fractures: Where a ligament or tendon pulls a piece of bone away from its attachment.
Taking Control of Your Knee Health
Understanding the posteromedial corner of your knee is essential for maintaining long-term joint health and preventing future problems. By recognizing potential risk factors, seeking prompt medical attention when needed, and actively participating in your treatment and rehabilitation, you can take control of your knee health and enjoy an active, pain-free life.
