Knee Deep in Innovation: How MRI and Magnetic Stem Cell Targeting Are Revolutionizing Cartilage Repair
"Discover how a groundbreaking study is using MRI to assess and improve magnetic stem cell therapy for damaged knees, offering hope for athletes and arthritis sufferers."
Knee pain, a familiar woe to athletes and those battling arthritis, often stems from cartilage damage. This resilient tissue, essential for smooth joint movement, lacks the inherent ability to heal itself due to its limited blood supply. As a result, even minor injuries can lead to chronic pain and reduced mobility. But, traditional treatments often involve invasive surgeries and extended recovery periods.
Fortunately, regenerative medicine offers a beacon of hope, particularly through stem cell therapies. Scientists have explored various methods of cartilage repair, with mesenchymal stem cells (MSCs) taking center stage. These cells, capable of differentiating into cartilage-producing cells, can be transplanted into damaged joints to stimulate healing. However, delivering MSCs effectively and ensuring their retention at the injury site has been a significant challenge.
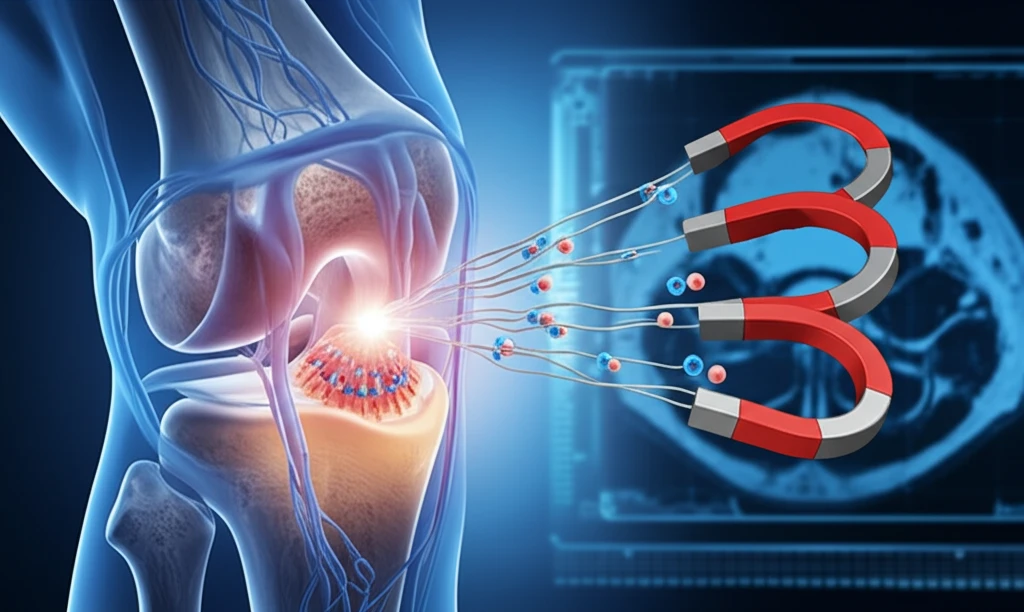
Now, imagine if we could guide stem cells directly to the damaged area using magnets. Recent research has made this a reality. A pioneering approach called magnetic stem cell targeting uses magnetic fields to deliver MSCs precisely to cartilage defects. A new study investigates the effectiveness of this method, combined with the power of magnetic resonance imaging (MRI) to monitor the repair process. The results are promising, offering new hope for those seeking less invasive and more effective cartilage repair options.
Magnetic Precision Meets Imaging Clarity
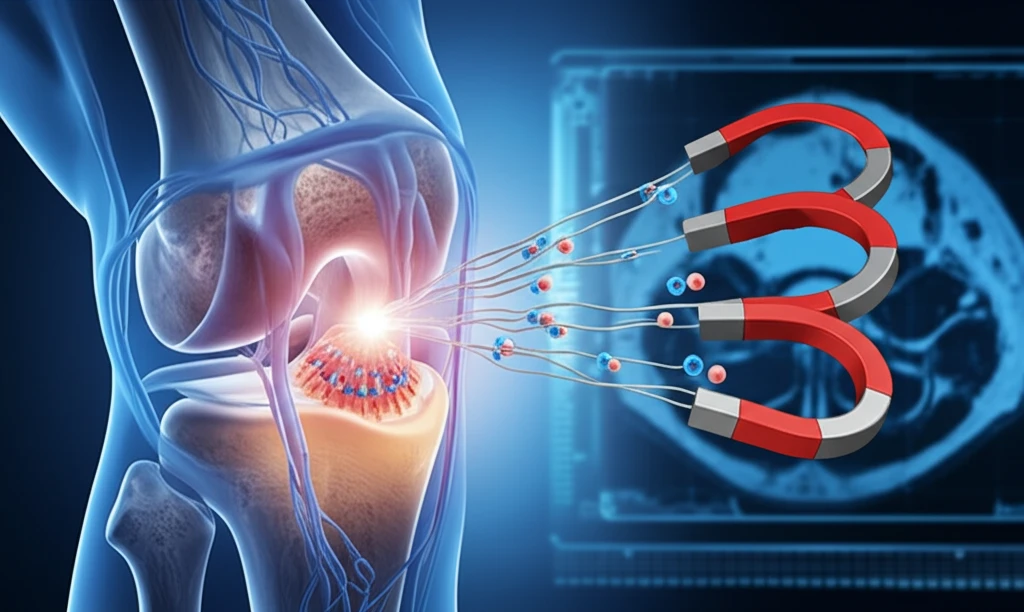
The study, published in Tissue Engineering, delves into the use of MRI to evaluate cartilage repair following magnetic delivery of stem cells. Researchers at Hiroshima University in Japan conducted a detailed experiment using rabbits to assess this innovative approach. They induced articular cartilage defects in the rabbits' knees and then treated them with magnetically labeled bone marrow mesenchymal stem cells (MSCs).
- T2 mapping of MRI successfully reflected the degree of cartilage repair, with the m-MSC group showing significantly better repair at 12 weeks.
- T2 images revealed hypointense areas in the m-MSC group, indicating the presence of iron particles from the magnetically labeled MSCs.
- Histological analysis confirmed the presence of iron particles in the repaired tissues at 1 and 4 weeks, but not at 12 weeks, suggesting their gradual metabolism.
The Future of Knee Care is Looking Up
This research marks a significant step forward in the field of regenerative medicine. By combining magnetic stem cell targeting with MRI evaluation, scientists have developed a powerful tool for assessing and improving cartilage repair. This innovative approach holds great promise for treating knee injuries and arthritis, offering patients less invasive and more effective treatment options. As research progresses, we can anticipate further refinements and broader applications of this technology, ultimately leading to improved outcomes and a better quality of life for those suffering from joint damage.
