Kidney Transplant Rejection: Unraveling Vascular Rejection for Better Outcomes
"A Deep Dive into Understanding and Managing Vascular Rejection in Kidney Transplant Patients"
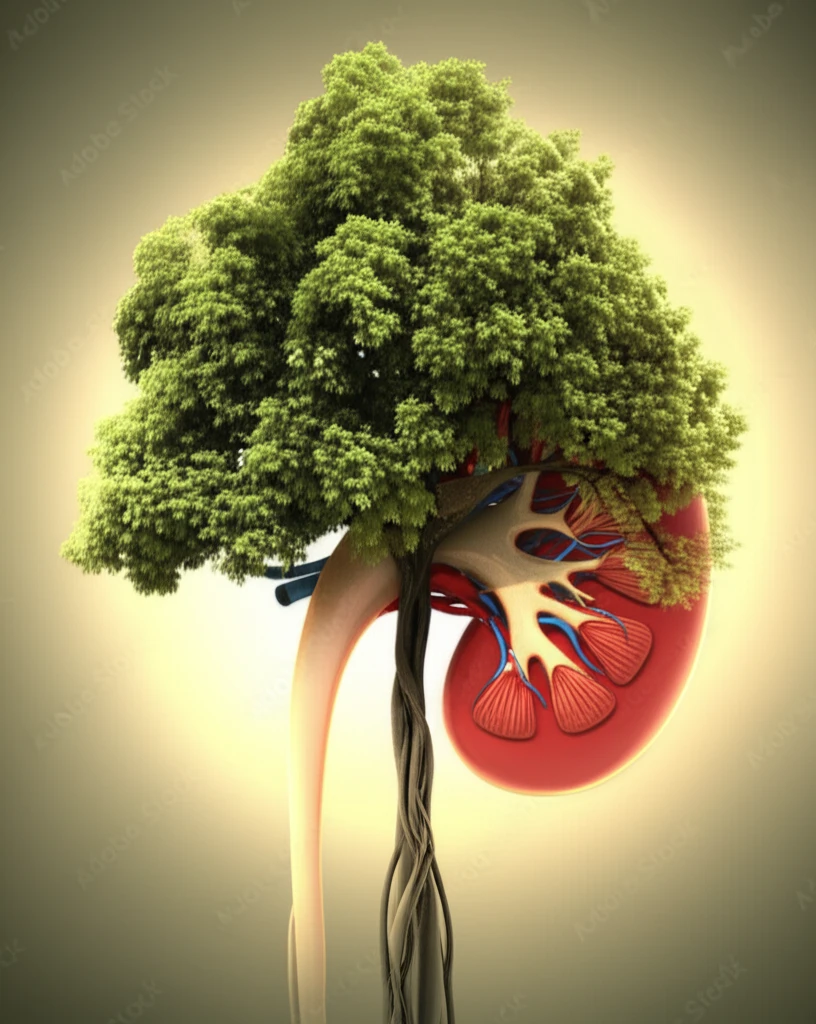
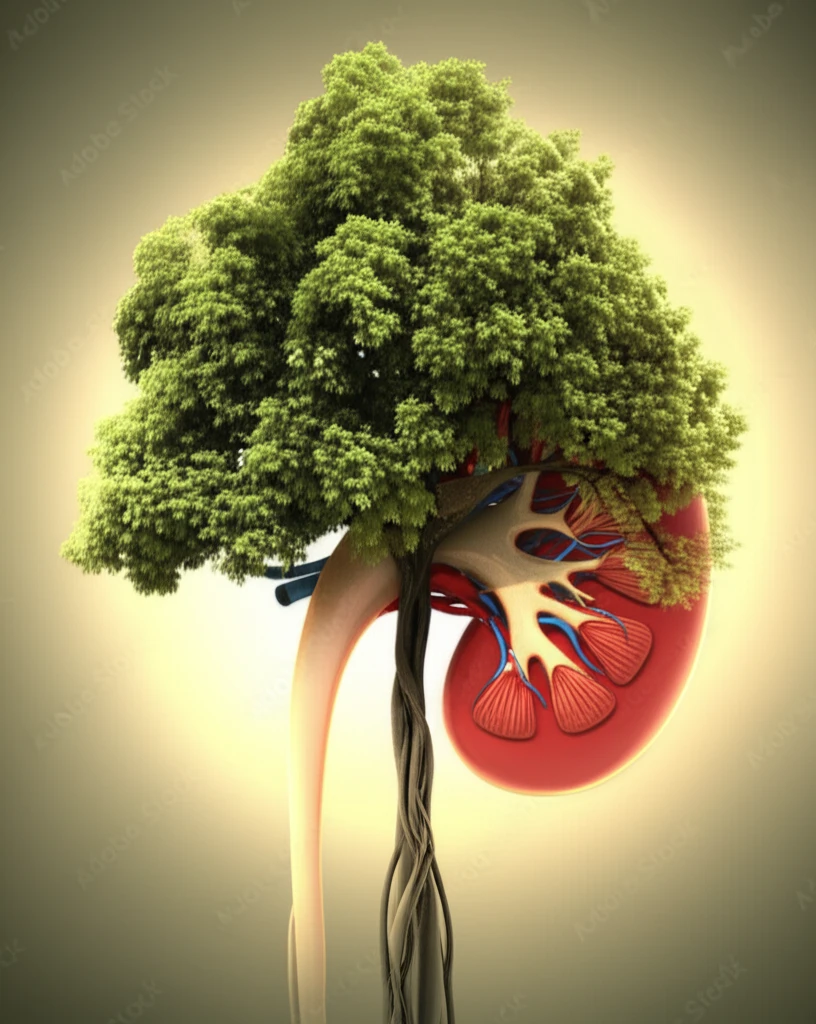
Kidney transplantation offers a new lease on life for individuals with end-stage renal disease. However, the journey doesn't end with the surgery. One of the most significant challenges post-transplant is the risk of rejection, where the recipient's immune system attacks the new kidney. Among the different types of rejection, acute vascular rejection (AVR) stands out as a particularly severe condition that can jeopardize the long-term survival of the transplanted organ.
Historically, AVR was primarily understood as a T-cell mediated process. However, contemporary research highlights the critical role of donor-specific alloantibodies (DSA) and their resistance to conventional treatments. This evolving understanding underscores the necessity for precise assessment of AVR phenotypes to enhance long-term prognosis and improve patient outcomes.
This article delves into the intricacies of vascular rejection in kidney transplantation, drawing upon a study that reviewed 940 patients to identify those who experienced AVR. We'll explore the different classifications of AVR, diagnostic approaches, treatment strategies, and the implications for long-term graft survival. By unraveling the complexities of vascular rejection, we aim to empower patients and their caregivers with the knowledge to navigate this challenging aspect of kidney transplantation.
Decoding Vascular Rejection: Types and Diagnosis
The study meticulously classified AVR into distinct categories based on histopathological findings and the presence or absence of DSA. These categories include:
- Isolated v-lesion (IV): Characterized by intimal arteritis (v) without other signs of rejection.
- T-cell mediated vascular rejection (TCMRV): Defined by severe tubulointerstitial inflammation (TI).
- Antibody-mediated vascular rejection (AMRV): Includes features of microvascular inflammation and C4d positivity with DSA.
- Suspected antibody-mediated rejection (sAMRV): Fulfills at least two out of three criteria for antibody-mediated rejection but may not have all the classic markers.
Navigating the Future: Treatment Innovations and Long-Term Outlook
The study's findings suggest that the low incidence of graft failure due to acute vascular rejection may be attributed to early detection, short follow-up periods, and intensive treatment protocols. However, the higher incidence of chronic rejection in AMRV and sAMRV groups underscores the need for continued vigilance and tailored management strategies.
Interestingly, the research revealed that some patients in the sAMRV group, despite exhibiting other features of AMR, did not have detectable DSA. This observation aligns with emerging evidence suggesting the role of non-HLA antibodies in vascular rejection, opening new avenues for research and potential therapeutic interventions.
Moving forward, a deeper understanding of the underlying mechanisms driving vascular rejection, including the role of non-HLA antibodies, is crucial for developing more targeted and effective therapies. By continuing to refine diagnostic approaches and treatment strategies, we can strive to improve long-term outcomes and enhance the quality of life for kidney transplant recipients.
