Kidney Recovery Breakthrough: Can We Prevent Chronic Kidney Disease After Injury?
"New research uncovers how stimulating a specific signaling pathway in kidney cells may prevent the progression of acute kidney injury to chronic kidney disease."
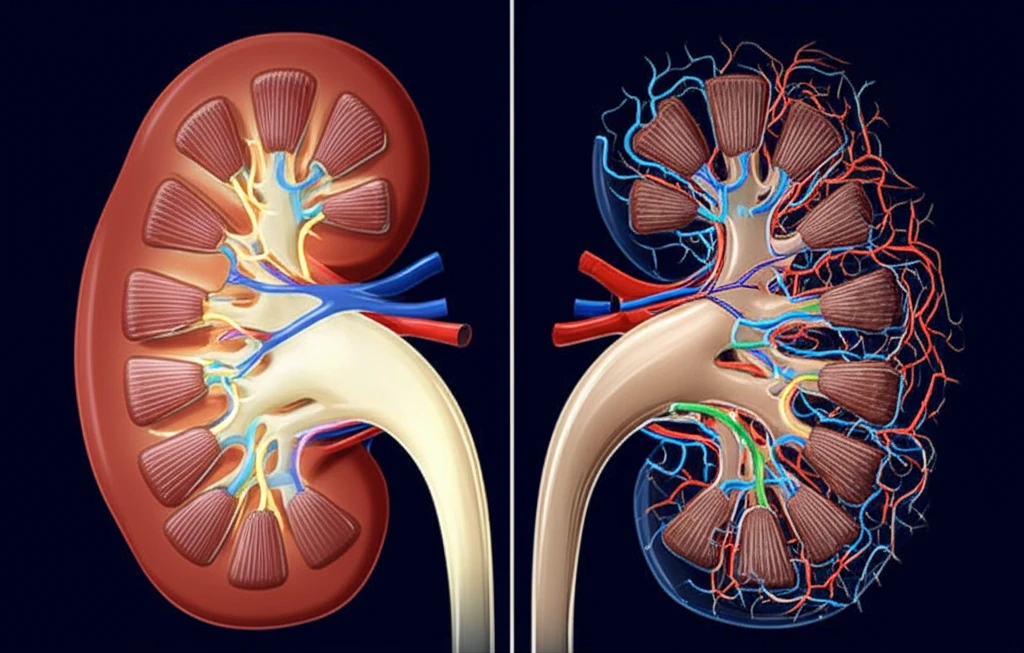
Acute kidney injury (AKI) is a serious condition that significantly increases the risk of developing chronic kidney disease (CKD). While kidneys possess a remarkable capacity for repair, severe or repeated AKI episodes can lead to maladaptive repair processes and the development of tubulointerstitial fibrosis, a hallmark of CKD.
Understanding the molecular pathways that determine whether the kidney recovers fully or progresses to chronic damage is crucial for developing effective treatments. Recent studies have focused on the bone morphogenetic protein (BMP) signaling pathway as a key player in this process.
A groundbreaking study published in Kidney International sheds light on how canonical BMP signaling in tubular cells can mediate recovery after acute kidney injury. Researchers have identified a specific mechanism that, when activated, helps prevent the progression of AKI to CKD, offering potential new therapeutic targets.
How Does BMP Signaling Work in Kidney Recovery?
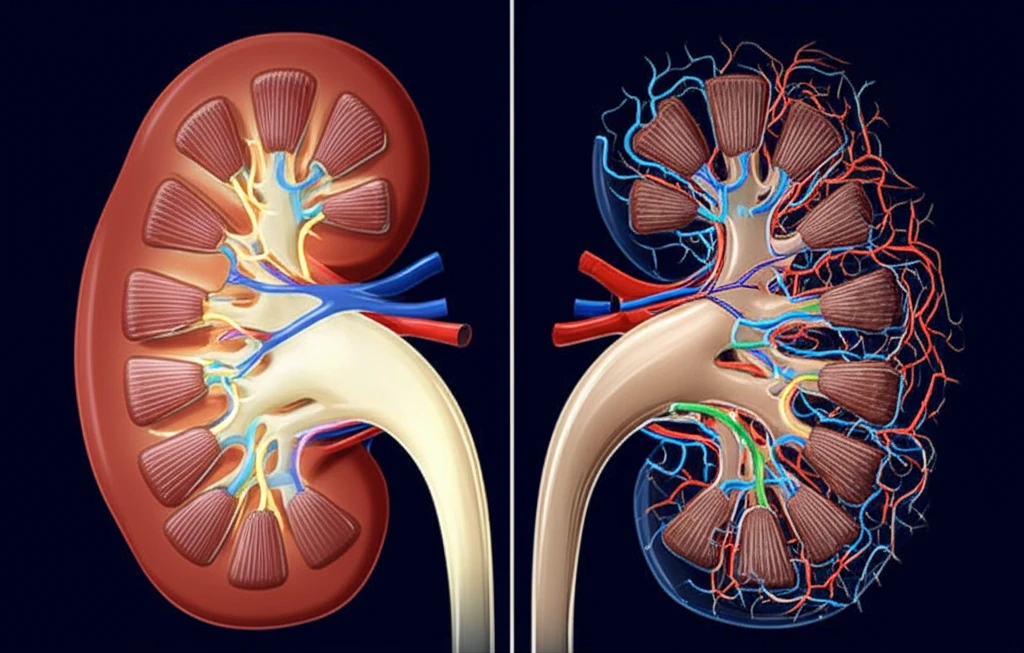
BMPs are part of the transforming growth factor-β superfamily and communicate by binding to type II BMP receptors. This initiates a cascade where type II receptors activate type I BMP receptors (BMPR1A and BMP receptor 1B), which then recruit and phosphorylate SMAD proteins (SMAD1, SMAD5, and SMAD8).
- Constitutive Activity: In healthy kidneys, canonical BMP signaling via SMAD1/5/8 is continuously active in renal tubules.
- Transient Downregulation: After an ischemic event, this signaling is temporarily reduced.
- Reactivation is Key: Successful tubular regeneration sees a reactivation of this BMP signaling.
A New Path Forward in Kidney Disease?
This research highlights the potential of harnessing the BMP signaling pathway to prevent the progression from AKI to CKD. By understanding and stimulating the mechanisms that promote kidney cell recovery, scientists hope to develop new therapeutic interventions that improve outcomes for individuals at risk of chronic kidney disease.
