Kidney Protection: Can We Prevent Damage from Hypoxia?
"New research highlights how targeting a specific protein could shield your kidneys from the harmful effects of oxygen deprivation."
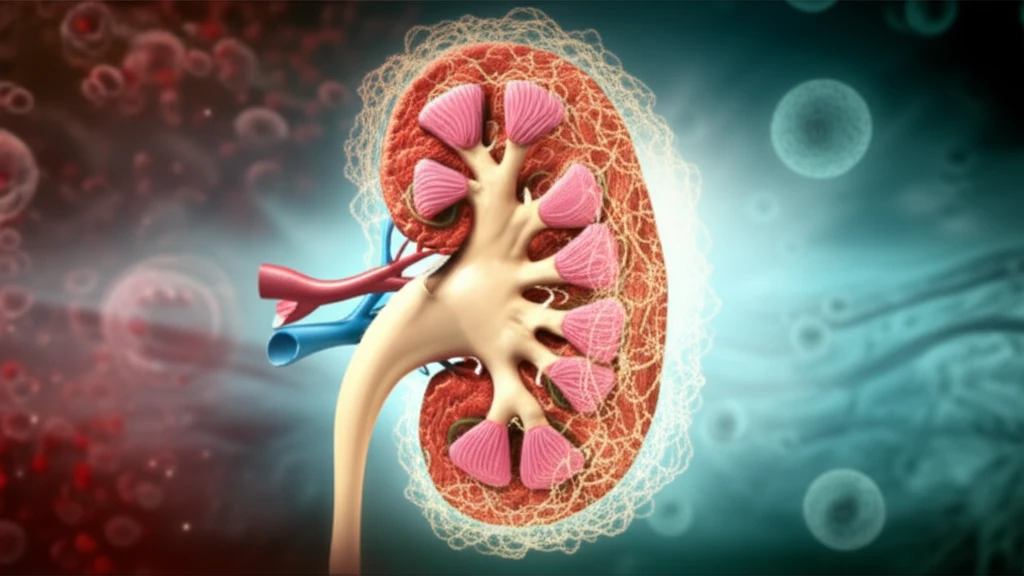
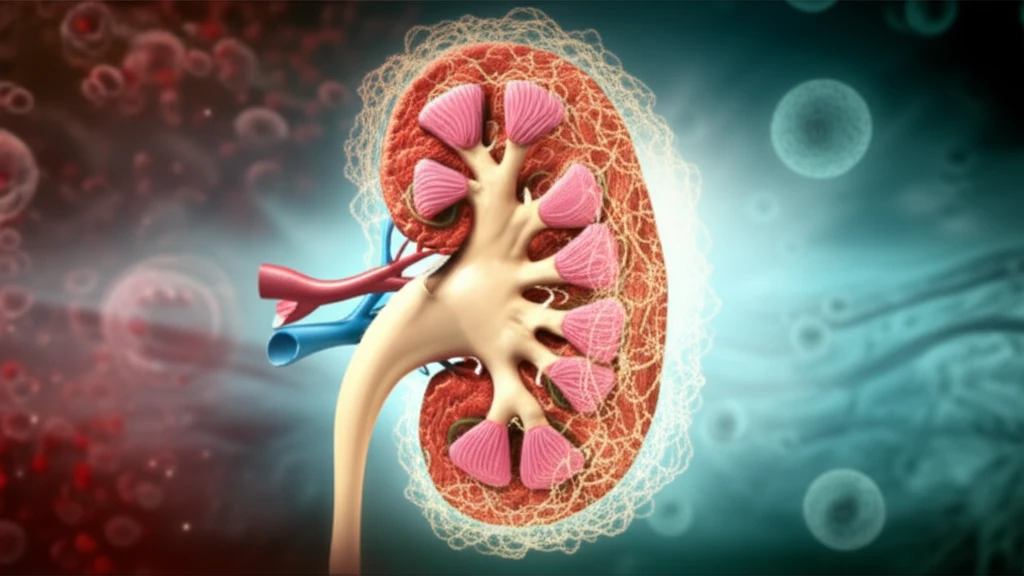
Acute kidney injury (AKI) is a serious condition that involves a rapid decline in kidney function, often requiring immediate medical attention. One of the major causes of AKI is ischemia-hypoxia, where the kidneys don't receive enough oxygen. This lack of oxygen can trigger a cascade of harmful processes, leading to significant damage.
The body has a natural response to low oxygen levels, primarily managed by a protein called hypoxia-inducible factor-1α (HIF-1α). HIF-1α helps the body adapt, but it's tightly controlled by another group of proteins called prolyl hydroxylase domain (PHD) proteins. Think of PHDs as the 'oxygen sensors' – they regulate how much HIF-1α is active. Among these, PHD2 is considered the most critical sensor.
New research explores whether inhibiting PHD2 could protect the kidneys during hypoxic events. By examining human kidney cells and a mouse model of ischemia-reperfusion injury (a process that mimics the oxygen deprivation and subsequent restoration seen in AKI), scientists are uncovering promising insights into kidney protection.
PHD2's Role: How Does Inhibiting It Help?
The study initially confirmed that when kidney cells (specifically, HK-2 tubular epithelial cells) were exposed to a chemical mimicking hypoxia (cobalt chloride, or CoCl₂), both PHD2 and HIF-1α levels increased. Interestingly, this exposure also led to increased cell death and activation of autophagy, a cellular 'self-eating' process that, while sometimes protective, can also contribute to cell damage.
- Autophagy Inhibition: Using a drug called 3-MA, they blocked autophagy. This protected the kidney cells from CoCl₂-induced damage, suggesting that in this scenario, autophagy was harmful.
- PHD2 Knockdown: They used siRNA to specifically reduce PHD2 levels in the cells. This also protected the cells from CoCl₂, potentially by increasing HIF-1α expression.
- HIF-1α Reversal: When they then reduced HIF-1α levels in the PHD2-inhibited cells, the protective effect disappeared, highlighting HIF-1α's crucial role.
- In Vivo Studies: Mice pretreated with a PHD inhibitor (L-mimosine) experienced less kidney damage from ischemia-reperfusion injury. The drug reduced cell death and inflammation in the injured kidneys.
The Future of Kidney Protection: What Does This Mean?
This research offers a promising new avenue for protecting kidneys from the damaging effects of hypoxia. By targeting PHD2, scientists may be able to develop treatments that reduce the severity of AKI and other kidney-related conditions. The study suggests that activating HIF, via inhibiting PHD, may be a useful therapeutic strategy in ischemic renal injury.
While these findings are encouraging, it's important to remember that this is early-stage research. Further studies are needed to fully understand the mechanisms involved and to determine the safety and effectiveness of PHD2 inhibitors in humans. The interplay between autophagy, apoptosis, and inflammation is complex, and more research is needed to fully elucidate the signaling pathways involved.
For individuals at risk of AKI (e.g., those undergoing major surgery, with chronic kidney disease, or with conditions like diabetes), these findings highlight the importance of managing risk factors and seeking prompt medical attention if kidney problems arise. As research progresses, new strategies for kidney protection may become available, offering hope for improved outcomes.
