Kidney Check: Do Stroke Treatments Put Your Kidneys at Risk?
"A closer look at contrast-induced nephropathy and stroke patients, balancing benefits and risks."
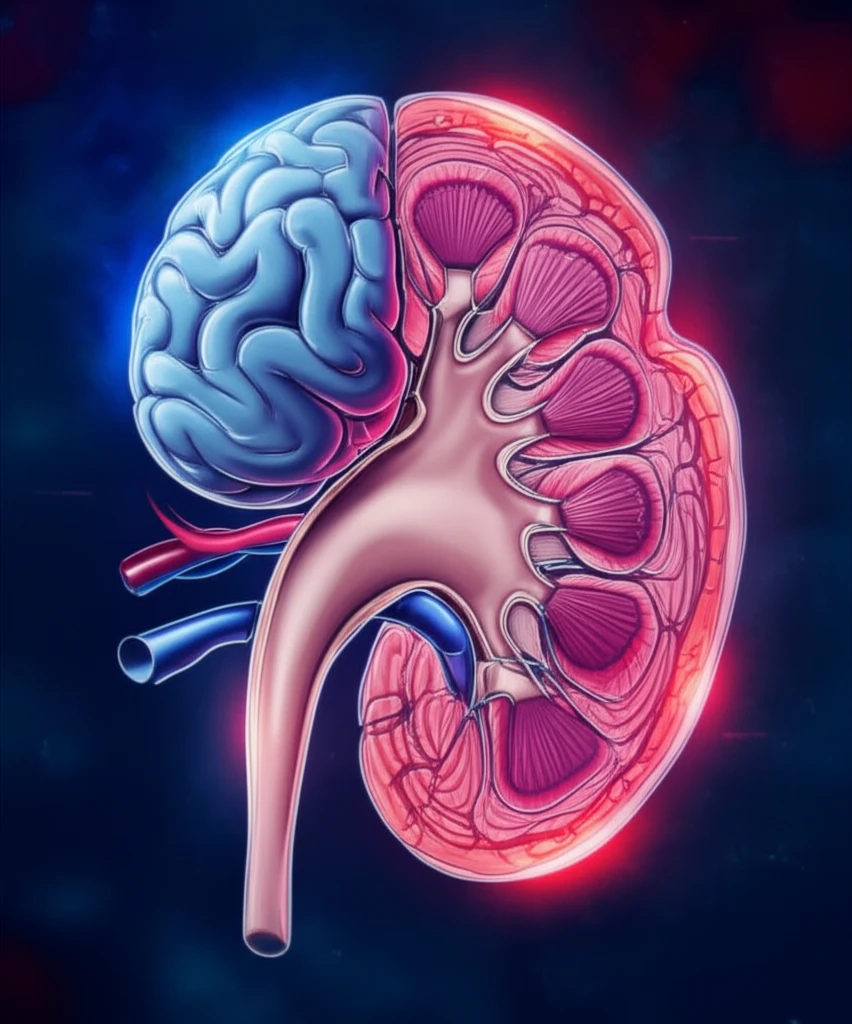
When someone experiences a stroke, quick action is essential. Doctors often use CT scans with contrast dye to see what's happening inside the brain, guiding them on how to treat the stroke effectively. However, there's a concern: can this contrast dye harm the kidneys, leading to a condition called contrast-induced nephropathy (CIN)?
A recent study by Brinjikji et al. investigated this very question, suggesting that the risk of kidney damage from contrast dye in stroke patients might not be as high as previously thought. This has sparked debate among experts, raising important points about patient safety and the best approaches to stroke care.
This article breaks down the discussion surrounding the study, exploring the nuances of kidney health in stroke treatment. We'll explore potential risks, offer practical insights, and empower you to understand the considerations involved in making informed decisions about stroke treatment.
Decoding CIN: What's the Real Risk for Stroke Patients?
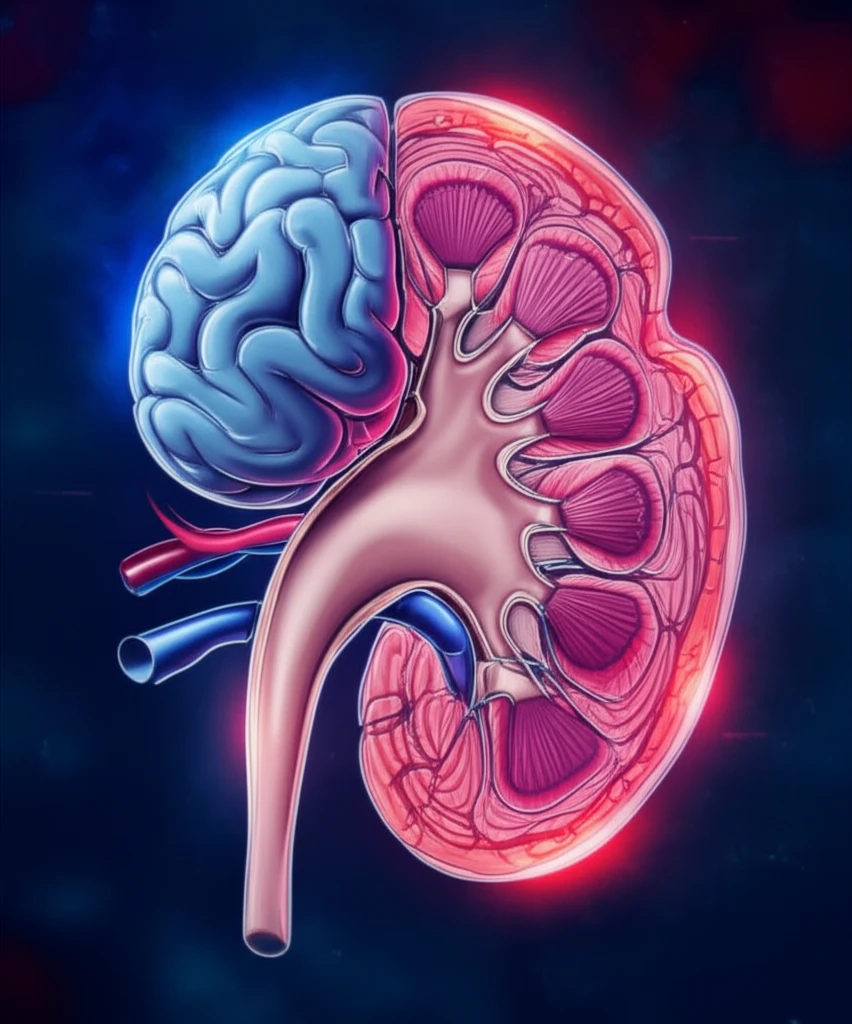
Contrast-induced nephropathy (CIN) is a decline in kidney function following exposure to contrast media, often used in imaging procedures like CT scans. Individuals with pre-existing kidney issues, diabetes, and heart failure are generally more susceptible. The challenge lies in balancing the diagnostic benefits of contrast-enhanced imaging with the potential risk of kidney damage, especially in the vulnerable population of acute stroke patients.
- Contradictory Findings: The meta-analysis revealed a lower AKI incidence in patients receiving contrast (2.3%) compared to those in case-controlled studies (6.3%).
- Pre-existing Conditions: Differences in baseline creatinine levels and risk factors like hypertension, diabetes, and heart failure among study participants raise questions about patient selection bias.
- Varied Definitions: Significant variability in AKI definitions across studies, along with inconsistent measurement timings (24-48 hours post-contrast), may not accurately reflect the extent of renal injury.
- Hydration Protocols: Only two studies specified standardized hydration protocols for patients receiving contrast, while none existed for the control group, potentially influencing CIN incidence.
The Takeaway: Proceed with Caution
While the study offers valuable insights, it's essential to interpret the findings with caution. The limitations within the included studies, such as variations in AKI definitions and hydration protocols, underscore the need for further research. Clinicians should carefully weigh the benefits and risks of contrast-enhanced CT scans on an individual basis, particularly in patients with pre-existing kidney conditions. By staying informed and prioritizing patient-centered care, we can ensure the best possible outcomes for individuals undergoing stroke treatment.
