Kidney Cancer and Lymph Node Invasion: What You Need to Know
"Debunking Myths About Tumor Location and Spread"
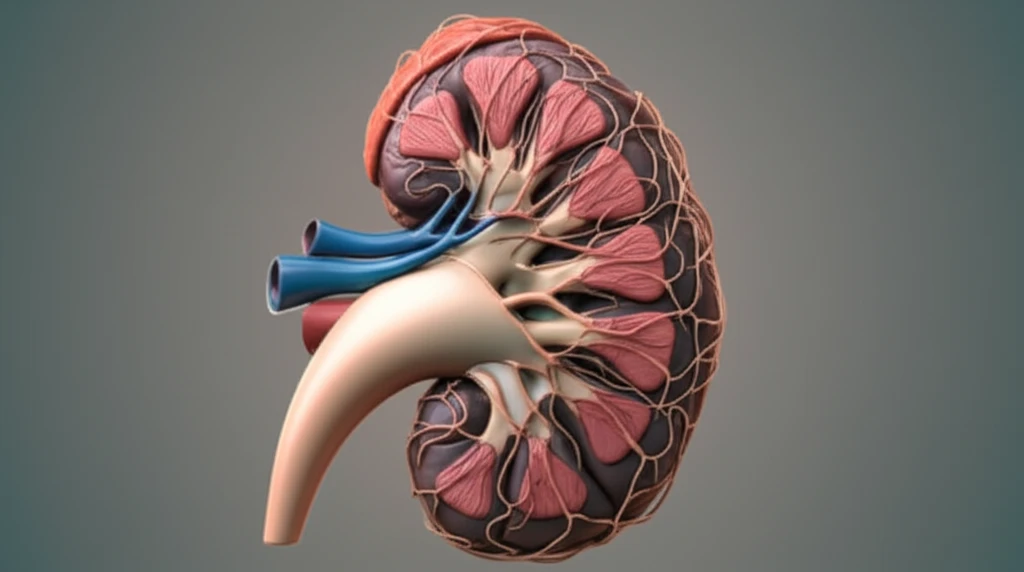
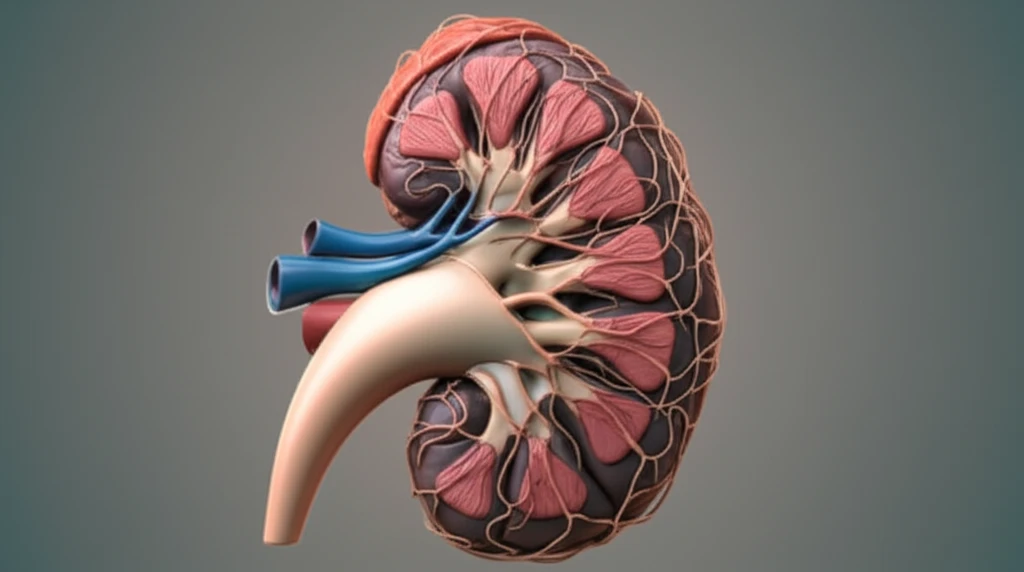
Kidney cancer is a formidable health challenge, and understanding its behavior is crucial for effective treatment. One of the critical aspects of managing kidney cancer involves determining if the cancer has spread to the lymph nodes, a process known as lymph node invasion (LNI). This information is vital for staging the cancer, planning treatment, and predicting outcomes.
Historically, there's been a decrease in performing lymph node dissections (LND) during kidney cancer surgery. This shift stems from a lack of definitive proof that LND improves cancer control, coupled with the rise of minimally invasive surgical techniques and stage migration—where cancers are detected earlier due to improved screening. However, accurate nodal staging remains essential for prognosis, follow-up schedules, and considering adjuvant therapies.
Adding to the complexity, past research using cadaveric dissections and sentinel-node studies has highlighted significant variability in how the lymphatic system drains from the kidneys. These studies have shown that the lymphatic vessels can reach retroperitoneal nodes or even connect directly to supraclavicular and mediastinal nodes, bypassing typical drainage routes. This unpredictability raises questions about whether the location of the primary tumor within the kidney affects the likelihood of lymph node involvement.
Does Tumor Location Really Matter?
A recent study published in the World Journal of Urology sought to clarify the role of tumor location and side in predicting lymph node invasion in renal cell carcinoma (RCC). Researchers analyzed data from 2,485 patients with unilateral RCC who underwent surgery at a single tertiary care center. The study aimed to determine if the side of the RCC (left versus right) and its location within the kidney (upper, middle, hilar, lower area, or multiple areas) influenced the risk of LNI or nodal progression (NP) during follow-up.
- Overall LNI and NP Rates: At the time of surgery, 15% of patients had LNI. During follow-up, 2.2% experienced nodal progression.
- Tumor Location and LNI/NP: Patients with tumors in more than one anatomical area of the kidney had higher rates of LNI and NP compared to those with tumors in a single area. Specifically, LNI rates were significantly higher in patients with tumors spanning multiple kidney areas (26%) compared to single areas (upper 11%, middle 10%, hilar 0%, lower 12%).
- Independent Predictors: Advanced disease characteristics such as cM1 (distant metastasis), cN1 (clinical lymph node involvement), pT2/pT3/pT4 stage (larger or invasive tumors), and high Fuhrman grade (3/4) were independent predictors of LNI and NP.
- Tumor Side and Location: Neither the side of the kidney with the tumor (left vs. right) nor the specific location of the tumor within the kidney independently predicted LNI or NP.
What Does This Mean for Patients?
The study's findings offer valuable insights for patients and healthcare providers. The reassurance is that the side of the kidney affected by cancer doesn't seem to influence the risk of lymph node involvement. However, tumors involving multiple areas of the kidney are associated with higher rates of LNI and NP, suggesting a more aggressive disease pattern. These results underscore the importance of comprehensive staging and tailored treatment approaches based on individual patient and tumor characteristics. By focusing on known predictors and understanding the nuances of tumor behavior, healthcare teams can optimize outcomes and provide the best possible care for individuals facing kidney cancer.
