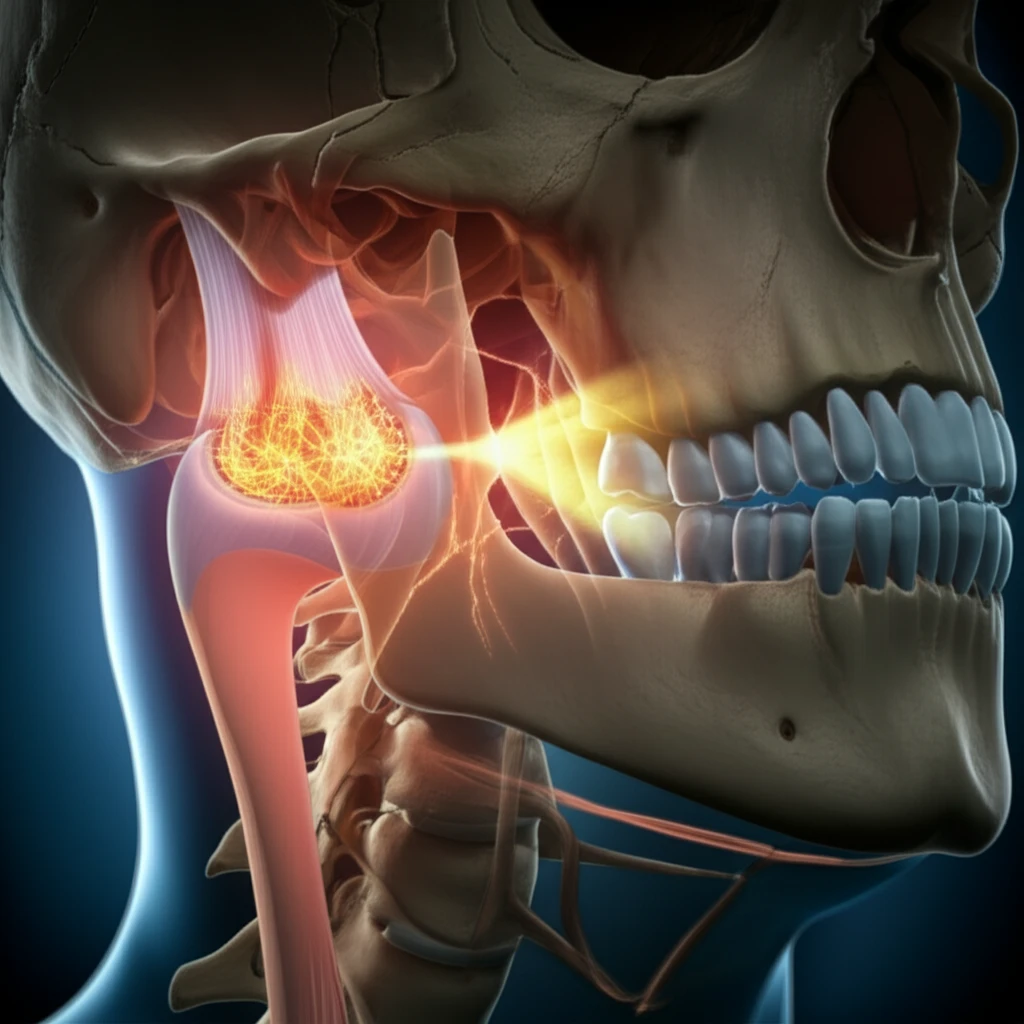
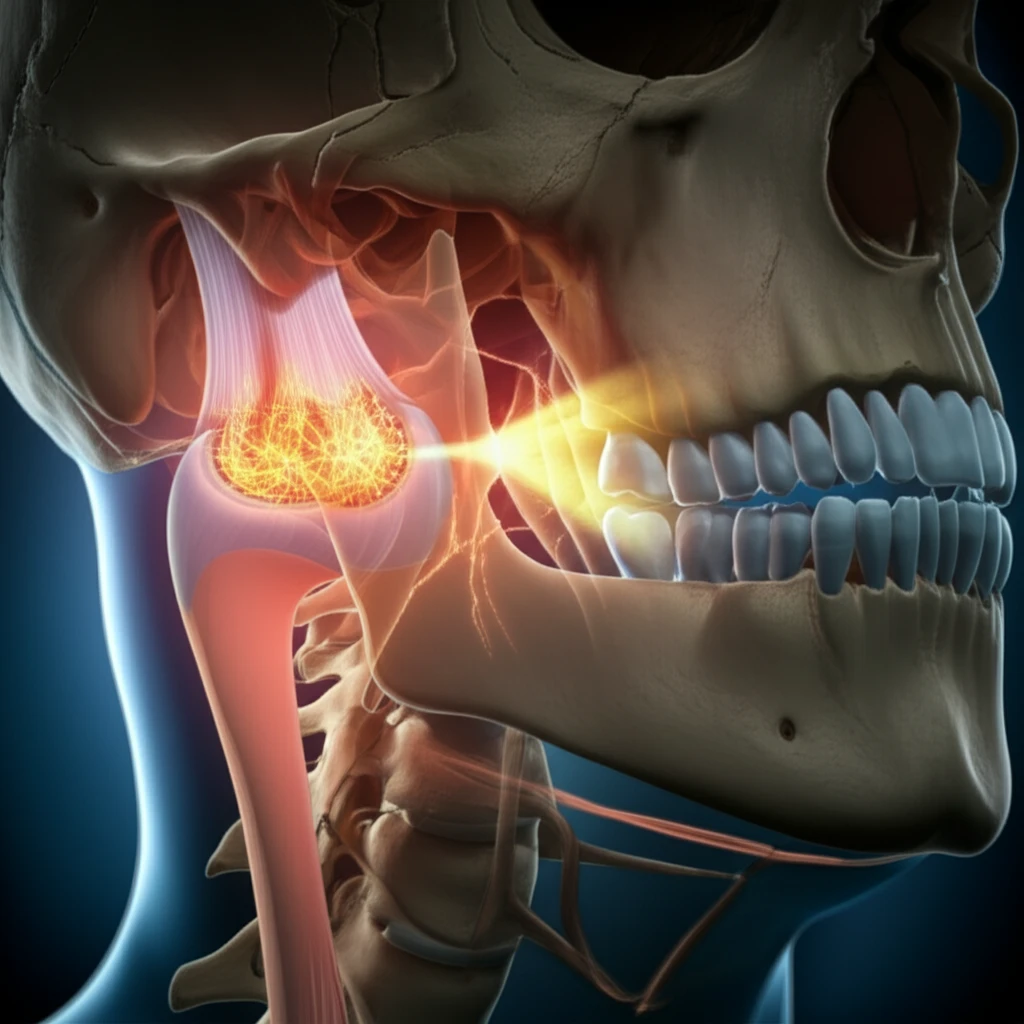
Jaw Osteoarthritis: Can Mechanical Stress Cause Bone Loss?
"New research reveals how mechanical stress on jaw cartilage can trigger bone loss, offering insights into TMJ disorders and potential treatments."
Temporomandibular joint osteoarthritis (TMJ-OA) stands out as a particularly challenging subtype of temporomandibular disorders (TMD). It's characterized by the breakdown of cartilage and changes in the underlying bone. While both cartilage degeneration and bone remodeling are hallmarks of TMJ-OA, the exact sequence of these events has been a subject of debate among researchers.
During skeletal development, chondrocytes—the cells found in cartilage—secrete various cytokines that influence bone formation and remodeling. However, the mechanisms through which chondrocyte signals prompt bone resorption (the breakdown of bone tissue) remain unclear. Understanding this process could unlock new therapeutic strategies for managing TMJ-OA.
Recent research has explored whether biomechanical stimulation of chondrocytes can promote osteoclastic bone resorption in the mandibular condyle, a key area affected by TMJ-OA. By understanding how mechanical forces influence these cells, we can pave the way for more targeted interventions.
The Link Between Mechanical Stress and Bone Resorption
A new study published in the Archives of Oral Biology (Kuang, Zeng, & Qin, 2019) aimed to determine whether biomechanically stimulated chondrocytes promote osteoclastic bone resorption in the mandibular condyle. The researchers subjected primary chondrocytes isolated from rat condylar cartilage to fluid flow shear stress (FSS) at varying intensities and durations. They then assessed the levels of pro-osteoclastic factors and the overall osteoclastic function.
- Increased Pro-Osteoclastic Factors: The study found that the mRNA and protein levels of SDF-1 and TGFβ-1 significantly increased in all FSS-treated groups. RANKL levels and the RANKL:OPG ratio also increased across all intensities and in longer durations of FSS (60 and 120 minutes). Wnt5A levels increased at all time points and in groups treated with higher FSS intensities (20 and 30 dynes/cm²).
- Correlation with Cartilage Degeneration: The percent area of degenerative cartilage changes was positively correlated with osteoclast number and osteoclast surface/bone surface in the mandibular condyles of rats with abnormal occlusion.
- Increased Expression in Abnormal Occlusion: Abnormal occlusion led to increased immune-positive areas and elevated mRNA expression levels of Sdf1, Tgfb1, Rankl, Wnt5a, and the RANKL:OPG ratio in rat condylar cartilage.
Implications and Future Directions
This research highlights the critical role of chondrocyte signaling in osteoclastic bone resorption within the mandibular condyle. The finding that mechanical stimulation can induce the expression of pro-osteoclastic factors by chondrocytes opens new avenues for therapeutic intervention in TMJ-OA. Future studies could focus on developing targeted therapies to modulate chondrocyte activity and prevent excessive bone resorption, ultimately improving outcomes for individuals suffering from this debilitating condition.
